The benefits of plant-based nutrition
This is the first article of a special 10 part series reviewing the essential nutrients needed for optimal health and the ability of plant-based diets to adequately meet recommendations.
March 31, 2023

Introduction
1 in 5 deaths globally (11 million in total) in 2017 were associated with poor diet.
This study looked at dietary intakes across 195 countries and quantified the burden of disease (population attributable fraction) that could be attributed to deaths related to cardiovascular disease, cancer, or type 2 diabetes, as well as the impact of diet on ill health (as disability-adjusted life-years or DALYs).
Table of contents
Benefits of Plant-Based Diets for Quality
Adequacy of Plant-Based Dietary Patterns
Nutrients of Public Health Concern
Overconsumed Nutrients
Other Nutrients of Interest
Nutrient Intake of US Adults
Key Points for Health Practitioners
Common Questions Regarding Plant Based Diets
Key Studies Supporting the Benefits of Plant Based Nutrition
Conclusion
Benefits of plant-based diets for quality
Though previously associated with undernutrition, poor diet is now often correlated with excess calories, saturated fats, trans fats, added sugars, and sodium.25-27 Overall, nutrition from plant-based diets is typically of higher quality than omnivorous diets, as assessed by the Alternative Healthy Eating Index (AHEI).28 A whole food plant-based (WFPB) diet is one made up of predominantly unprocessed fruits, vegetables, whole grains legumes, nuts and seeds, and excludes animal foods, with certain selective supplementation of vitamins B12. Sometimes D. Intentionally planned, WFPB diets provide sufficient nutrient intakes for all stages of life and can be therapeutic for chronic disease and overall health and healing.29 The plant-based dietary pattern protects against overconsumption of nutrients that lead to obesity and disease,30 particularly animal protein, saturated fat,31 trans-fats, cholesterol simple sugars,32 and sodium.33, 34
Adequacy of plant-based dietary patterns
The following sections discuss achieving appropriate intakes of specific nutrients from food and certain necessary supplements in the context of a whole food, predominantly plant-based dietary pattern. Deficiencies can be dangerous but are also preventable through nutrition. Adequate intake is necessary, but supplementation may lead to excess and may be harmful to some people.35
Macronutrients
All macronutrients (protein, carbohydrate, and fat) are present in whole plant foods in varying proportions. No individual food is equivalent to a particular macronutrient.
Protein
Though protein is typically associated with animal foods in the U.S., predominantly plant-based and entirely plant-based diets easily meet or exceed recommended protein intake.29 The RDA for protein is .8 grams per kg of body weight or 10–11% of calories taken in. For instance, to calculate requirements for a person weighing 150 pounds (68.2kg), multiply 0.8 (g protein) by 68.2 (kg). This equates to ~55 g protein daily. Each gram contains 4 calories: 55 grams of protein multiplied by 4 (calories per gram) = 220 calories, which is 11% of calories in a 2,000 calorie/day dietary pattern for most individuals. Some populations, including the elderly, some athletes, and those healing from diseases, may need higher amounts. Older adults may need 1.0 to 1.3 grams per kg of body weight per day.36 Protein intakes in the American diet are typically higher than this amount, and failing to meet this RDA is unlikely except in cases of energy malnutrition (insufficient calories).
In the body, proteins are broken down by enzymes into their amino acid building blocks and built into proteins as needed.37 The nine essential amino acids (leucine, isoleucine, methionine, phenylalanine, histidine, tryptophan, valine, threonine, and lysine) are synthesized only by plants. They must be obtained from food or supplements to build all other amino acids (alanine, β-alanine, asparagine) and peptides.38 With sufficient caloric intake, adequate levels of essential amino acids are supplied throughout the course of a day to meet requirements.29 Regular intake of legumes also provide other essential nutrients, as well.29 Though all whole plant foods have protein, rich sources include soy products, legumes, nuts and seeds.39 Whole grains are a source of proteins, with sprouted grains having increased protein content.40
Fat
Those consuming a plant-based diet are more likely to achieve a healthy fat intake than most omnivorous diets. Fat requirements are very low, and plant foods are able to supply all essential fat requirements. The AIs for linoleic acid (LA, an omega-6 fatty acid) is only 12 grams per day for adult women under 70 years and 17 grams for men under 51 or 14 grams for those 51–70 years. AI for alpha-linolenic acid (ALA, an omega-3 fatty acid) is 1.6 grams/day for adult males and 1.1 grams for adult females.41
Fatty acids serve many vital roles, including the facilitation of normal metabolism, absorbing fat-soluble vitamins, producing hormones and other essential compounds, and controlling inflammation.42 Both omega-3 (n-3) and omega-6 (n-6) fatty acids are needed. Most individuals consume much more n-6 polyunsaturated fat than n-3, largely from vegetable oils (found in most processed foods) and also meat, poultry, fish, and eggs. Dietary intakes of ALA, the precursor to n-3 fatty acids eicosatetraenoic acid (EPA) and docosahexaenoic acid (DHA) include cold-water fish and seafood. Flaxseed, soybeans, walnuts, and leafy green vegetables are also good sources.39 A tablespoon of flaxseed has 3 grams of fat with 2.35 grams ALA.
Humans convert both essential fatty acids to longer-chain fatty acids using the same desaturation enzymes. The n-3 fatty acid (ALA) is converted to DHA and EPA, and the n-6 (LA) is converted to arachidonic acid (AA). N-3 and n-6 compete for the same desaturation enzymes, and a high intake of LA appears to interfere with the desaturation and elongation of ALA.43
The ratio between n-6 and n-3 fatty acids may be important, and a ratio of 1:1 to 2:1 is consistent with evolutionary aspects of diet as well as neurodevelopment and genetics.44 Their balance may bean important determinant in brain development and decreasing the risk for cardiovascular disease, hypertension, cancer, diabetes, arthritis, and other autoimmune and possibly neurodegenerative diseases.44
Plant-based eaters generally have lower blood levels of EPA and DHA, and these nutrients may be virtually absent in vegans.45 Those with higher needs or reduced conversion ability may receive some benefits from supplementation.5 Though deficiency in dietary fat is rare if sufficient calories are consumed, some conditions may put patients at risk, including eating disorders, large bowel obstruction, or metabolic disorders. Whole food sources of healthy fats include nuts, seeds, avocados, and olives.46 Half an avocado contains roughly 11 grams of fat, one ounce of almonds or sunflower seeds has 14 grams, a handful of olives (5) has roughly 2 grams of fat, and 1 cup of plain tofu has 11.86 grams of fat.47 However, whole grains, legumes, and vegetables also contain varying fat levels; given such low requirements, unrefined whole plant foods easily supply sufficient quantities.
Refer to the Saturated Fat section under “Overconsumed Nutrients” for more information on saturated fat and health risks.
Carbohydrates
Whole foods with unrefined, complex carbohydrate from legumes, vegetables, whole grains, and fruits are the best options for health and caloric needs and are associated with positive health outcomes.48 The RDA of carbohydrates for children and adults is 130 grams per day.41 A diet based on whole, unrefined plant foods is likely to be relatively higher in carbohydrate as a percent of total calories than typical American dietary patterns.
Refined carbohydrates such as white bread, added sugars, and polished rice or corn are associated with negative health outcomes, including overweight, obesity, metabolic disorders,49 heart disease,50 and type 2 diabetes51 and should be discouraged.48 Found in processed food, refined carbohydrates make up the bulk of carbohydrates consumed by Americans.52,53
Public health concern
The following sections describe plant food sources of specific nutrients and background information on each nutrient.
Calcium is found in many plant foods. Though cow’s milk is often touted as the best source, our bodies may absorb calcium from plant foods at a higher rate. The RDA for calcium is 1,000 mg/day for most adults and 1,200 mg/day for women over 50.41 Dairy foods have a 30% bioavailability, whereas some plant foods, though they contain less calcium, have a higher absorption rate.54, 55 For example, bok choy contains 160mg of calcium per 1 cup but has a bioavailability of 50%, thus 80 mg is absorbed.55 Even though totally plant-based diets theoretically contain enough calcium to meet RDAs, nearly half of all Americans do not meet the EAR for calcium.
Plant sources of calcium are adequate to meet needs. For example, calcium-set tofu has the same calcium availability as cow’s milk.56 Plant-based sources of calcium include bok choy, broccoli, Brussels sprouts, kale, collard greens, tofu, winter squash, and almonds.55, 57 Foods high in calcium include tofu prepared with calcium sulfate, soybeans, enriched cornmeal, and fortified plant milks, as well as dairy products. Vegetables, particularly those low in oxalates, are good sources of calcium (greens such as kale, or collard greens).47
Potassium is easily found in many plant foods and is needed for blood pressure regulation and bone health; thus, lower intake is associated with cardiovascular, renal, and bone health risks.58, 59 The AI for adults 19–70 is 2,600 mg/day for women and 3,400 mg/day for men.41 Lower intake of fruits and vegetables in the Western diet has led to decreased potassium intake.60, 61 The regulative effect of potassium on acid-base balance is one hypothesis for its effects on bone health and the prevention of osteoporosis. Further, dietary potassium may reduce kidney stones and slow the progression of kidney disease from renal vascular, tubular, and glomerular damage. It may also help to suppress renal inflammation.60 Potassium’s hypertensive effects include the decrease in intravascular volume. Though there is an established relationship between potassium and chronic disease, it is difficult to establish a proven lowest level of intake to prevent disease, and, thus, there is yet to be a specific potassium CDRR.62 There is an association between white vegetable consumption and decreased risk of stroke.58 Potatoes are the highest sources.58 Other foods rich in potassium include yams, avocado, and most varieties of beans.47 Fruit and vegetable sources include banana, beet greens, apricots, and dates,63–65 as well as nuts, green vegetables, yogurt, chickpeas, and tuna.63, 65, 66
Dietary fiber is found exclusively in plant foods. The AI for fiber is 14 g per 1,000 calories per day,3 which translates to 25 g per day for women <50 yrs and 21 g for those >50 yrs. For men, it is 38 g <50 yrs and 30 g for >50 yrs.41 On average, American adults consume half the recommended amount of fiber.67 A predominantly plant-based diet rich in whole foods allows for plenty of fiber in the diet.29 Foods high in fiber include black beans, split peas, lentils, avocado, raspberries, dried figs, flaxseeds, oatmeal, and whole wheat pasta. Other fiber-rich foods include blueberries, strawberries and other fruit, winter squashes, brown rice, whole-grain bread, popcorn, mushrooms, almonds or peanuts, and sunflower or sesame seeds.47 Though it does not contribute to our energy needs, fiber is essential to gut health and immune function and helps control pathogens, as well as being a protective factor for many chronic diseases.
Vitamin D, or calcitriol, is an exception to the list of nutrients provided completely by plant food sources in that it is a fat-soluble steroid hormone produced endogenously from sun exposure. It can be consumed from some foods, as well as provided by fortified foods or supplements.68 The RDA for vitamin D is 15 mcg/600IU up to 70 years old and 20 mcg/800 IU above 70 years.3, 68
Sunlight is a better source of vitamin D than dietary sources as ultraviolet (UV) B radiation transforms the precursor of vitamin D in the skin into vitamin D3. Usually, adequate vitamin D levels can be synthesized internally if large areas of the body, including the face, arms, legs, back, or chest, are exposed to direct sunlight between the hours of 10am–3pm; without sunscreen for five to 30 minutes at least two days a week. Those with darker skin pigmentation require more extended amounts of time in the sun.68, 69 Supplemental sources of vitamin D may be required to meet needs in the cases of insufficient synthesis, including for those on a plant-predominant diet, and especially in winter seasons or for individuals who have limited exposure to the outdoors.70 Foods high in vitamin D include fortified milks, both dairy and non-dairy, fortified juice, fortified cereals,3, 63 salmon, or high fat fish,3, 63 and mushrooms treated with ultraviolet light.71 Vitamin D may be provided by eggs as well as mushrooms that are treated with or exposed to ultraviolet light, as well.72
The importance of vitamin D is indicated by the predominance of vitamin D receptors throughout the body. The two primary forms, D2 (ergocalciferol) and D3 (cholecalciferol), only differ in their side chain structures. The small intestine absorbs both forms. As a vitamin, it regulates body calcium levels, phosphorus, and bone mineralization, and controls cellular proliferation and differentiation. Vitamin D also regulates gene expression in specific tissue73 and protects against oxidative stress from its antioxidant properties.
It is assumed that most people do not make enough D from sun exposure due to indoor living. Deficiency can result in brittle bones, rickets, osteomalacia,73 and/or osteoporosis.74 Symptoms of low vitamin D include fatigue, bone, joint, or muscle pain, and anxiety. In addition, studies suggest that low vitamin D levels can be linked to diabetes and insulin resistance, high blood pressure, multiple sclerosis, and possibly some cancers.73, 75[us_separator size=”small”][vc_column_text el_id=”over-consumed-nutrients”]
Overconsumed nutrients
Added Sugar: Excess intake of added sugars is associated with weight gain, excess body weight and obesity, type 2 diabetes, high serum triglycerides, higher cholesterol, high blood pressure and hypertension; stroke; coronary heart disease, cancers, and dental caries.52 The recommendation in the 2020 Dietary Guidelines for Americans is to limit added sugar intake to no more than 10% of calories.3 A whole food diet that avoids refined grains and prepared foods is naturally low in added sugars. Naturally occurring sugar in whole food, such as fruits, is not associated with adverse health effects. On the contrary, foods with naturally occurring sugars have consistently been found to be protective against disease and are not associated with harmful health outcomes.76
Sodium: The ubiquitous intake of processed foods has led to an excess in sodium intake. The CDRR is <2,300 mg/day. Most adults in the U.S. consume more than 3,400 mg each day.77 Though the body needs very small amounts of sodium to function, evidence points to an association with excess salt consumed and elevated blood pressure levels, a major risk factor for cardiovascular disease.78 The food groups that are highest in salt are generally those that are commercially prepared. Almost 50% of dietary salt intake comes from mixed dishes defined by the USDA Dietary Guidelines as: “burgers, sandwiches, and tacos; rice, pasta, and grain dishes; pizza; meat, poultry, and seafood dishes; and soups.”26 Limiting consumption of commercially processed foods is an important strategy to reduce excess sodium intake. Focusing on whole foods and preparing meals at home naturally avoid excess sodium consumption.
Saturated Fat: The 2020–2025 USDA dietary guidelines have, again, called for Americans to cut their saturated fat intake to under 10%,3 and the American Heart Association recommends a dietary pattern that achieves 5%-6% of calories from saturated fat,79 which is naturally achieved by eating an entirely plant-based diet.80 Current U.S. intake is 11%.3 Because they are found primarily in animal foods, plant-based diets are naturally low in saturated fats, which are associated with risk of cardiovascular disease and diabetes.80–82 Saturated fats have been shown to increase LDL-C,83 a known causal factor in atherosclerosis,84 through the development of lipoproteins that promote foam cell formation, part of the fatty streak phase of atherosclerosis. These deposits in the arterial wall initiate an inflammatory response.85 Further, in epidemiologic and metabolic studies, saturated fat has been associated with insulin resistance and oxidative stress.86–88 Research has found that individuals eating vegetarian-type dietary patterns have lower saturated fat and cholesterol intakes, and unsaturated fat intake appears to be relatively similar between plant-based and non-plant-based eaters.45, 89, 90
Other nutrients
Vitamin B12 or cobalamin is a group of complex molecules with a single cobalt atom at their center. B12 is one of the eight B vitamins making up the water-soluble vitamins, which are absorbed easily into the bloodstream. The RDA for vitamin B12 is 2.4 mcg/day, which is easily consumed through fortified foods or supplementation.3, 41, 68, 91
Vitamin B12 is made by microorganisms found in the soil and water, as well as produced by microorganisms in the intestines of animals. Vitamin B12 is stored in the liver and muscle tissue, so it is naturally found in animal foods and not plant foods. The amount made in the intestines is not adequately absorbed, so it is recommended that people consume B12 in food or supplementation. Though essential, humans need very small amounts of vitamin B12 to achieve adequate intake (2 to 3 milligrams a day). Because the body can store cobalamin for up to three years, it can take several years for deficiency to present.91
Vegetarians and the elderly have a high risk of vitamin B12 deficiency due to low consumption, as well as lower absorption.92 Other factors unrelated to age or diet may influence B12 absorption, including intestinal damage and acidity levels (lack of hydrochloric acid in the stomach and increased acidity in the small intestine).93 Medications such as proton pump inhibitors and H2 blockers prescribed for GI disorders like GERD can inhibit absorption. Pancreatic insufficiencies of intrinsic factor (IF) production, which is required for the transportation and absorption of vitamin B12, will also result in lower uptake of B12.94 Acidification of the small intestine, parasites, or bacterial growth in the gut can inhibit absorption, as well.93 Plant-based eaters have lower average circulating concentrations of vitamin B12 and a higher risk for elevated homocysteine levels and developing clinical symptoms related to B12 deficiency, including unusual fatigue, tingling in the fingers or toes, poor cognition, poor digestion, and failure to thrive in small children.95, 96 Thus, there is a need for supplementation for those eating an entirely plant-based diet (no animal foods at all) for several years, as well as for older adults.
Magnesium is needed for many chemical reactions in the body as well as for neuromuscular connections. The RDA for magnesium is 310 mg for females <30 yrs and 320 mg for >30 yrs, and 400 mg for males <30 yrs and 420 mg for >31 yrs.41 Most people obtain enough from diet, though green leafy vegetables, whole grains, nuts, and fish are good sources.97 Other sources of magnesium include tofu, potatoes, yogurt, and meat, or tuna.47
Vitamin A is vital for cell reproduction and differentiation, immune function, and good vision. It comes from two sources: plant sources provide carotenoids, and animal sources provide retinol. The RDA is 700 μg /day for adult women and 900 μg/day for adult men.41 Because it can be toxic in high supplemental doses, there is a UL of 3,000 μg/day for adults.98 Foods high in retinol (the vitamin A1 found in food and supplements) include cooked sweet potato or spinach, raw carrots, cantaloupe, or butternut squash. Beef liver is very high in vitamin A. Other foods containing vitamin A include dairy, plant milks, and fortified cereals.
Vitamin C or L-ascorbic acid is required to turn fat into energy and make collagen. It is needed to create certain neurotransmitters and is involved in protein metabolism.99 The RDA for vitamin C is 75 mg for adult women and 90 mg for adult men.41 Foods high in vitamin C include bok choy, parsley, daikon radish, broccoli, cantaloupe, Brussels sprouts, pineapple, cabbage, cauliflower, mustard greens, papaya, green peas, kale, tomatoes, strawberries, turnip greens, orange, guava, kiwi, mango, and red pepper. Other sources include spinach, most other leafy green vegetables, including collard greens, celery, and fruits, including cherries, pears, and canned peaches.47
Vitamin E refers to a collection of fat-soluble compounds with distinctive antioxidant properties. They protect cells from the damaging effects of unstable free radicals that can damage cells and can contribute to cardiovascular disease and certain cancers.100 The RDA for vitamin E is 15 mg/day for adults.41 Foods high in vitamin E include sunflower seeds, almonds and hazelnuts, sunflower and safflower oils, and trout. Other foods containing vitamin E include peanut and olive oils, corn oil, and peanut butter.47
Iodine is an essential component of the two thyroid hormones, thyroxine and triiodothyronine, which regulate many biochemical functions, including protein synthesis and enzyme activity.101 It is a trace element found in soil and the sea and, thus, obtained from plants and sea vegetables.102 The RDA for iodine is 150 μg/day for adults and more for pregnant and lactating women,97 with a UL of 1,100 μg/day.3, 103 Levels above 2 mg/day can impair hormone function and stimulate acne.104 Iodine is also in meat and dairy, as animals eat food grown in soil. Though essential, its only known function is as a component of thyroid hormones. These hormones regulate cell growth and activity, particularly important to the nervous and skeletal system development.105
Dietary iodine sources can vary widely in the U.S.,106 and iodine intake among plant-based eaters can be low for those who do not consume sea vegetables or iodized salt; supplementation may be needed.106 Iodine deficiency was common in the early 20th century, with goiter being epidemic. Deficiency can also impair mental development and promote cognitive impairment.107 In the U.S., iodization of salt began in the 1920’s. By the 1970’s, the U.S. population had excessive iodine intake, sometimes leading to hyperthyroidism or autoimmune thyroiditis.107 High iodine intake is more common now than deficiency and can occur from excessive dairy intake. Iodine is used as a sterilizer for milking machinery and teats and as a supplement in dairy cow feed. Iodine is also used as dough conditioners in baked goods. Deficiency is found in areas where the soil is deficient, e.g., from glacial runoff or flooded plains. A majority (75%) of the sodium consumed in the U.S. is not iodized, particularly coming from processed foods. Sea vegetables are considered a good source. Skins of tubers, such as potatoes, have iodine, as well.104, 105
Iron is needed to build hemoglobin for red blood cells to carry oxygen from lungs to body tissue. It is vital to muscle function and ATP energy production and as a cofactor for several enzyme systems. The RDA for iron is 18 mg/day for adult women under the age of 51 and 8 mg/day for older women, as well as all adult men,3 though RDAs for vegetarians are 1.8 times higher than for meat-eaters, as heme iron from meat is more bioavailable than nonheme iron from plant-based foods, and meat, poultry, and seafood increase the absorption of nonheme iron.108 Iron deficiency is one of the most common nutritional deficiencies, particularly in women and children. Low levels can lead to anemia, though not necessarily due to poor diet. Blood loss from ulcers, colitis, diverticulosis, heavy menstrual bleeding (menorrhagia), and microscopic bleeding is associated with anemia.109, 110 Though vegetarians generally consume as much iron as non-vegetarians, their iron stores are typically lower, which may be advantageous unless suffering from malnutrition. Excess circulating ferritin, the protein that contains iron, has been associated with a higher risk of developing metabolic syndrome,111 heart disease, cancer, and premature aging.108 Heme iron found in meat is more readily absorbable than non-heme iron, found in plant foods, which is more tightly regulated by the body. Because iron is a pro-oxidant, excess iron can increase free radical production that can damage tissues. Polyphenols in coffee and tea can reduce iron absorption, while vitamin C can increase absorption. Iron is plentiful in legumes, grains and beans, and fruits and vegetables. Cow’s milk has very little iron and may inhibit absorption.112 Iron deficiency is not typically found among vegetarian populations; however, vegetarian women have been shown to have a higher prevalence of anemia (Hb <120 g/L),113–115 and absorption of iron in the context of mixed diets is typically more influenced by iron status than by the type of iron (heme vs. non-heme).116
Zinc is a mineral and is found in the soil and sea. Like most minerals (calcium being the exception), the body only needs small amounts, which easily accumulate. It competes for transporters with other minerals, so absorption is affected by the balance of other minerals (iron, manganese, nickel, calcium, and phosphate). The RDA for zinc is 8 mg for adult women and 11 mg for adult men.41 Zinc is involved in many functions, including brain cell communication, hemoglobin activity, male reproductive cell function, night vision, immunity, and wound healing.104, 105 Its absorption is partly dependent on the supply of vitamin B6, and, like any nutrient, environmental variables can affect it, particularly oral contraception or hormone replacement use and heavy metal (mercury, lead, and cadmium) interference.104 Further, zinc (as well as copper and iron) is found to be present in the beta-amyloid plaques formed in the brains of Alzheimer’s patients. Studies indicate that it may encourage these proteins to clump together into plaques. So it may be that these metals work together in this disease, encouraging plaque. Dietary sources of zinc include legumes, seeds, nuts, wheat and corn, soy products, as well as animal food sources.105, 117
Choline, a water-soluble vitamin, is now recognized as an essential nutrient needing established dietary reference values. The AI for choline is 425 mg for adult women and 550 mg for adult men, with a UL of 3,500 mg.41 Choline is important for the nervous system as the precursor to the neurotransmitter acetylcholine. It is also involved in cell structure, lipid transport, and cognitive development during pregnancy.57 The requirements for choline have partly been informed by studies in women and men who developed liver damage upon becoming deficient.118, 119 Choline is found predominantly in animal foods, though there are several plant-based sources with lower amounts, including beans, tofu, green vegetables, potatoes, nuts, seeds, whole grains, and fruits.47 High choline intake is associated with increased risk of cardiovascular disease from the production of TMAO by gut microbiota120 and prostate cancer.121 Egg, broccoli, and chickpeas are good sources of choline.47
Nutrient intake of US adults
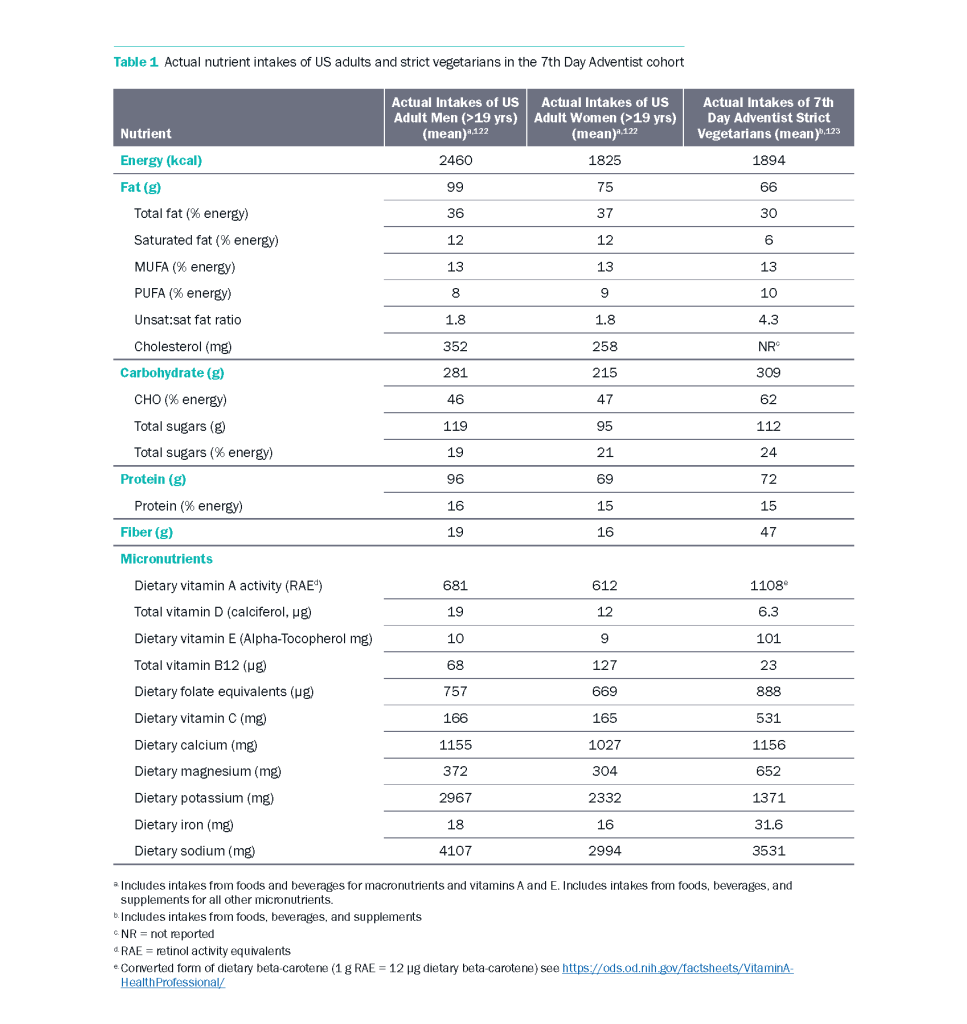
Table 1 displays mean nutrient intakes from US adults, using the What We Eat in America data (National Health and Nutrition Examination 2015–2018) for men and women in comparison to mean intakes among strict vegetarians (completely plant-based/vegan) in the 7th Day Adventist cohort. Striking contrasts are visible for both macro and micronutrients, as well as certain similarities, such as the % protein intake. The mean nutrient intakes of the strict vegetarian group demonstrate the feasibility of plant-based diets to provide adequate nutrient intake.
Key points for health practitioners
Diet quality should be a concern for all regardless of the parameters of the specifics of an individual’s diet. To examine the nutritional quality of plant-based diets, we extracted information on 13 studies examining nutrient status and overall diet quality of plant-based diets—WFPB, vegan, vegetarian, and lacto-ovo-vegetarian (LOV) diets. Studies are detailed in Appendix Table 1. Of the studies extracted,3 were randomized controlled trials (RCTs),134–136 one was an observational cohort study,137 two were cross-sectional,95, 138 and three were systematic reviews and/or meta-analyses,89, 139–141 and one examined theoretically derived dietary patterns.70 Studies examined overall dietary quality, omega-3 (n-3) fatty acid intake and levels, magnesium status, vitamin D and calcium intake, vitamin B12 and folate levels, zinc intake, and iron status.
For n-3 fatty acids, one study examined whether retroconversion of DHA to EPA was a viable method for replacing seafood intake in maintaining n-3 levels.134 The authors estimated that rates of retroconversion in vegetarians were approximately 9.4% DHA to EPA compared to just over 1% in previous studies, suggesting a significant retroconversion of DHA to EPA in humans.
In studies that examined magnesium intake in vegans,141 it was found that vegans had higher magnesium consumption than meat-eaters and that red blood cell content of magnesium was not statistically different between groups. In addition, pregnant subjects from the same study reported fewer calf cramps on a plant-based diet compared to meat-eaters. One study examining theoretically derived diet plans found that a WFPB diet may contain 70% more magnesium compared to diet plans based on USDA MyPlate.
It is well-known that plant-based diets often lack vitamin B12, especially if individuals refrain from consuming fortified foods. One cross-sectional study found that vegans had significantly lower serum concentrations of vitamin B12 but higher folate levels compared to meat-eaters.95 These findings highlight the necessity of plant-based individuals to supplement with vitamin B12, consume B12 fortified foods, or both.
As discussed, vitamin D is a Nutrient of Public Health Concern. Consumption and serum levels of vitamin D are lower on plant-based diets than omnivorous diets, as animal foods contain vitamin D.135, 136, 138 Individuals should consider incorporating fortified sources of vitamin D into their plant-based diets in addition to meeting RDAs for calcium consumption. Multiple studies found that calcium intake was lower in individuals on plant-based diets,70 except with one study that found an increase in calcium consumption with a tailored whole food, plant-based diet intervention.135 Finally, zinc and iron are nutrients of interest for plant-based and nonplant-based individuals alike, as studies extracted found decreases in serum zinc and increases in zinc excretion associated with pregnancy in both groups,140 and vegans and vegetarians were found to have lower iron intakes and iron stores in one meta-analysis.141
At the same time, plant-based diet interventions have consistently shown improvements in diet quality. One theoretical analysis found that WFPB diet adherence could lead to increased vitamin A activity, vitamin E, folate, vitamin C, magnesium, potassium, and iron while lowering saturated fat and added sugar consumption.70, 89, 136 In terms of food components, WFPB diets could lead to more than a doubling in vegetable, legume, whole fruit and grain, and nut and seed consumption.70, 89, 136 In addition, observational and intervention studies alike consistently find significant increases in dietary quality indices such as the Healthy Eating Index and Alternative Healthy Eating Index compared to baseline and individuals following control diets, including American Diabetes Association guidelines.89, 135, 136
Well-planned plant-based diets can lead to significant improvements in dietary quality and provide a framework for individuals to adjust lifestyle factors to prevent chronic conditions like obesity, hypertension, cardiovascular disease, and type II diabetes. However, these diets should be well planned to meet nutrient requirements and should be high in vegetables, fruits, whole grains, legumes, nuts and seeds, and other whole plant foods. Supplements for vitamin B12, and as needed, vitamin D, should be incorporated.
Common Questions Regarding Plant-Based Diets
Will I get enough protein on a plant-based diet?
Meeting protein requirements happens easily on an entirely or predominantly plant-based diet if consuming enough calories. Theoretical models of the nutrient composition of WFPB diets have calculated 16% energy from protein compared to the USDA MyPlate, which was calculated at 19% protein from mixed animal and plant sources.70 Research including the comprehensive China Study indicates consumption in excess of human requirements may promote disease.124, 125
Will I get enough calcium and iron on a plant-based diet?
Though plant foods contain phytates that inhibit iron, zinc, and calcium absorption, the estimated intake of these minerals in theoretical nutrient compositions of whole food, plant-based diets exceeded the RDA, except for calcium in women over 50 years.70 Unfortunately, nearly half of Americans do not even meet the EAR for calcium, despite the majority of them consuming an omnivorous diet.122 Fruit and vegetable intake may help in absorption by shifting pH towards base. Caffeine and alcohol may inhibit absorption modestly by increasing excretion of calcium.126
Will I be at risk for anemia?
Anemia indicates a reduced level of red blood cells from decreased production, blood loss, or destruction of red blood cells. Iron deficiency is the most common cause of anemia, and menorrhagia is the most common cause of blood loss.116 Iron is an essential protein of hemoglobin in red blood cells that carry oxygen in the blood and myoglobin that provides oxygen to muscles. Since iron absorption is determined by the amount present in the body (circulating and stored), and the modulation effect of both inhibitors and enhancers to absorption of dietary iron, the amount of iron absorbed varies depending on the food taken in at each meal, the composition of the overall diet, and individual iron status. When iron stores are low in the body, absorption from food is higher, and visa-versa.116 It is important to note that meat and vitamin C from fruits and vegetables enhance the absorption of iron,127 and that cow’s milk and dairy products might inhibit absorption due to their calcium,128 and from their protein casein.129
Plant-based eaters need to take in adequate amounts of vitamin C from food, as well as vitamin B12 from supplementation, in order to maintain optimal iron status. Vitamin B12 is necessary to produce new red blood cells, which carry oxygen throughout the body. The B vitamin folate is also necessary for the production of red blood cells. Sufficient intake of these nutrients has been correlated with adequate serum ferritin levels, the circulating protein that contains iron. Ferritin is what is used to measure iron stores.115
In some studies, vegetarians have been found to have a higher prevalence of depleted iron stores, as well as higher incidence of iron deficiency anemia, particularly in premenopausal vegetarian women.115 Other studies have shown that serum ferritin and hematocrit levels of vegetarians were similar to non-vegetarians.114 Helicobacter pylori infections can also leave people at risk for deficiency.130 Healthful sources of iron include greens and legumes, and a diet including these as well as fortified grains can easily provide adequate iron. The CDC recommends that iron supplementation be individualized based on hemoglobin and hematocrit screenings, as well as medications taken.131
Will I get enough vitamin D on a plant-based diet?
Humans are designed to obtain most vitamin D from sunlight, and many individuals who spend most or all of their time indoors may fall short of requirements. Vitamin D is not naturally widespread in food but is mostly in animal products, particularly fish and egg yolks. Mushrooms also contain vitamin D, and if left out in the sun, they can absorb more.132 Foods fortified with vitamin D in the United States include cow and soy milk, orange juice, and certain breakfast cereals.
Will I get enough B12 on a plant-based diet?
Supplementation will be necessary. Vitamin B12 (and possibly vitamin D) are the exception to the overriding understanding that a whole food, plant-based diet provides all nutrients needed for a health promoting diet. This vitamin is not widely in soil or water as it once was, and therefore supplementation is advised for vegans. Animals produce it in their lower intestines, so meat and dairy products may be sources, but nutritional deficiency can occur in plant-based populations and the elderly.133
Supporting the benefits of plant-based nutrition
Diet quality should be a concern for all regardless of the parameters of the specifics of an individual’s diet. To examine the nutritional quality of plant-based diets, we extracted information on 13 studies examining nutrient status and overall diet quality of plant-based diets—WFPB, vegan, vegetarian, and lacto-ovo-vegetarian (LOV) diets. Studies are detailed in Appendix Table 1. Of the studies extracted,3 were randomized controlled trials (RCTs),134–136 one was an observational cohort study,137 two were crosssectional,95, 138 and three were systematic reviews and/or meta-analyses,89, 139–141 and one examined theoretically derived dietary patterns.70 Studies examined overall dietary quality, omega-3 (n-3) fatty acid intake and levels, magnesium status, vitamin D and calcium intake, vitamin B12 and folate levels, zinc intake, and iron status.
For n-3 fatty acids, one study examined whether retroconversion of DHA to EPA was a viable method for replacing seafood intake in maintaining n-3 levels.134 The authors estimated that rates of retroconversion in vegetarians were approximately 9.4% DHA to EPA compared to just over 1% in previous studies, suggesting a significant retroconversion of DHA to EPA in humans.
In studies that examined magnesium intake in vegans,141 it was found that vegans had higher magnesium consumption than meat-eaters and that red blood cell content of magnesium was not statistically different between groups. In addition, pregnant subjects from the same study reported fewer calf cramps on a plant-based diet compared to meat-eaters. One study examining theoretically derived diet plans found that a WFPB diet may contain 70% more magnesium compared to diet plans based on USDA MyPlate.
It is well-known that plant-based diets often lack vitamin B12, especially if individuals refrain from consuming fortified foods. One cross-sectional study found that vegans had significantly lower serum concentrations of vitamin B12 but higher folate levels compared to meat-eaters.95 These findings highlight the necessity of plant-based individuals to supplement with vitamin B12, consume B12 fortified foods, or both.
As discussed, vitamin D is a Nutrient of Public Health Concern. Consumption and serum levels of vitamin D are lower on plant-based diets than omnivorous diets, as animal foods contain vitamin D.135, 136, 138 Individuals should consider incorporating fortified sources of vitamin D into their plant-based diets in addition to meeting RDAs for calcium consumption. Multiple studies found that calcium intake was lower in individuals on plant-based diets,70 except with one study that found an increase in calcium consumption with a tailored whole food, plant-based diet intervention.135 Finally, zinc and iron are nutrients of interest for plant-based and nonplant- based individuals alike, as studies extracted found decreases in serum zinc and increases in zinc excretion associated with pregnancy in both groups,140 and vegans and vegetarians were found to have lower iron intakes and iron stores in one meta-analysis.141
At the same time, plant-based diet interventions have consistently shown improvements in diet quality. One theoretical analysis found that WFPB diet adherence could lead to increased vitamin A activity, vitamin E, folate, vitamin C, magnesium, potassium, and iron while lowering saturated fat and added sugar consumption.70, 89, 136 In terms of food components, WFPB diets could lead to more than a doubling in vegetable, legume, whole fruit and grain, and nut and seed consumption.70, 89, 136 In addition, observational and intervention studies alike consistently find significant increases in dietary quality indices such as the Healthy Eating Index and Alternative Healthy Eating Index compared to baseline and individuals following control diets, including American Diabetes Association guidelines.89, 135, 136
Well-planned plant-based diets can lead to significant improvements in dietary quality and provide a framework for individuals to adjust lifestyle factors to prevent chronic conditions like obesity, hypertension, cardiovascular disease, and type II diabetes. However, these diets should be well planned to meet nutrient requirements and should be high in vegetables, fruits, whole grains, legumes, nuts and seeds, and other whole plant foods. Supplements for vitamin B12, and as needed, vitamin D, should be incorporated.
Conclusion
Though diet quality is intrinsically linked to disease etiology and health outcomes, the typical American diet lacks the micronutrients needed for optimal health. Excess energy contributes to disease epidemics, including cardiovascular diseases, metabolic diseases including diabetes, many cancers, and decreased quality of life. Whole food, plant-based diets address these problems of nutrition adequacy and excess by providing all nutrients necessary (with the possible exception of vitamins B12 and D) without excess calories and foods that promote increased risk for chronic disease.
CONTINUE READING IN THIS SERIES
Acknowledgement
This review was made possible in part due to a generous donation from Kate Farms. For more information on Kate Farms please visit their website here. www.katefarms.com
Take the Next Step
Ready to turn knowledge into action? Gain practical tools and skills to support plant-based nutrition for your patients and community:
- Our Food as Medicine Jumpstart Guide is free, comprehensive PDF packed with tips, meal ideas, and actionable strategies to help patients get started with plant-based eating.
- Our Culinary Medicine Program is a dynamic, self-paced online program designed to help clinicians translate the science of nutrition into practical skills patients can use in the kitchen..
Empower yourself and your patients with the skills to make lifestyle change practical, achievable, and delicious.