The Benefits of Plant-Based Nutrition: Treatment and Prevention of Reproductive Cancers
Whole food, plant-based diets may decrease risk for reproductive cancers and potentially reduce rates of reoccurrence. Evidence on plant-based diets can be communicated to patients to support their ability to make informed decisions course of treatment.
Abstract
As the number of centenarians increases globally due to improved living standards and access to quality healthcare, efforts to improve quality of life through modifiable health behaviors are even more relevant for the lifestyle medicine (LM) practitioner. Avoidance of the chronic diseases that plague our society today prolongs life and circumvents premature mortality1–7 while also making living better, not just longer, possible. Research indicates that a plant-based diet is the cornerstone of healthy longevity and potentially the most important prescriptive tool to help patients achieve a longer life and better quality of life as they age.
Key Points for Practitioners
- Whole food, plant-based diets have utility both in decreasing risk for reproductive cancers as well as potentially reducing rates of reoccurrence
- Important elements of plant-based diets that seem to reduce cancer risk include the reduction or elimination of animal protein and fat, the presence of fiber, and the high concentration of antioxidants
- Whole food, plant-based diets have no adverse side effects and are associated with other health benefits such as cardiometabolic health, healthy weight, and longevity
- Existing evidence on plant-based diets and cancer can be communicated to patients to support their ability to make informed decisions about their diet and course of treatment
- With appropriate care and planning, plant-based dietary interventions are complementary to conventional cancer treatments
- When weight loss is a concern, calorie tracking or plant-based enteral formulas may be helpful
- If patients express interest in trying a whole food plant-based diet of some kind, it is helpful to share educational and support resources with them
Abstract
A whole food, plant-predominant diet offers benefits for risk reduction. It also complements conventional treatment of reproductive cancers by supporting healthy weight, reducing inflammation, potentially reducing insulin-like growth factor (IGF-1), increasing glucose tolerance, and increasing consumption of antioxidants to prevent oxidative damage. Reducing consumption of meat and dairy, saturated fat, and animal protein; increasing fiber consumption; maintaining normal hormone levels; and altering the gut microbiota also offer benefits of a whole food, plant-based (WFPB) diet to reduce cancer risk. Practitioners can support patients in adopting a plant-based diet by providing dietary prescriptions and educational resources for successful dietary transitions and maintenance.
Reproductive Cancers in Context
Cancer is characterized by uncontrolled cell growth and proliferation,1 and it is the second leading cause of death in the US.2 Cancer types are typically named for the organs or tissues of origination.1 For women, reproductive cancers include cervical, ovarian, endometrial (uterine), vaginal, vulvar, and breast cancers,3 of which only cervical cancer has an early detection screening test.
Although breast is the most common reproductive cancer among women, ovarian is the deadliest, with a 5-year survival rate of only 44%, as early detection is difficult. Only 15% are diagnosed in stage 1, where the survival rate is 92%.
More than 20,000 cases in the U.S. were diagnosed in 2020.4 Fallopian tube cancer can occur but is very rare.5 For men, reproductive cancers primarily include testicular, penile, and prostate cancers.3 Survival rates for the last two male cancers are 98% and 95%,6 respectively. This paper will focus on the most common reproductive cancers in the US, including breast, endometrial, prostate, and testicular cancers.
Causes and Risk Factors
According to the American Cancer Society, common causes of cancer include smoking and tobacco use, diet and physical activity, exposure to the sun and other types of radiation, as well as certain viruses and other infections.7,8 While some risk factors are unmodifiable (sex, age, adult attained height, or genetics), other risk factors are potentially modifiable.8 These are primarily related to lifestyle and include smoking, alcohol consumption, diet, and physical activity. Dietary risk factors include red and processed meat consumption, under-consumption of fruits and vegetables, dietary fiber, and dietary calcium.8
Some reproductive cancers have known causes with high attributable risks,8 while others are less certain . For instance, the sexually transmitted human papillomavirus (HPV) is the known cause of cervical cancer, and the increased risk of this cancer is linked to early sexual behavior, multiple sexual partners, and exposure to other sexually transmitted infections .9 Conversely, the causes of breast10 and endometrial11 cancers are less certain and likely multifactorial with strong associations established, while risk factors include hormonal, lifestyle, and environmental factors, age, comorbidities (e .g ., obesity, type 2 diabetes), and the patient’s personal and family health histories. While the causes of prostate and testicular cancers are also unknown, risk factors include age, race, and family history.12,13 Obesity is an additional risk factor for prostate cancer,12 and undescended testicle and abnormal testicle development are additional risk factors for testicular cancer.13
Treatment and Outcomes
Despite medical advances and successful treatments, cancer is a leading cause of death in every country globally and is the first or second leading cause of death before age 70 in nearly 60% of all countries.14 Common cancer treatments include invasive surgeries, chemotherapy, and radiation . Less common treatments involve targeted immunotherapy, laser, hormonal, and other treatments, including some experimental.15 Treatment options and prognoses vary by the type of cancer, stage, tumor size at diagnosis, the site(s), and extent of metastasis.16 Further, individuals respond differently to treatments, and patient comorbidities can reduce or complicate the efficacy of treatment options. It is also important to note that many available treatments are costly and can cause unpleasant or fatal side effects. Therefore, the best way to avoid the risks involved in treatment and the debilitating and deadly outcomes associated with cancer is through prevention and risk reduction.
Prevention and Early Detection
According to the World Cancer Research Fund and the American Institute for Cancer Research (WCRF/ AICR), an estimated 30-50% of all cancer cases are preventable through healthy lifestyle practices and avoidance of carcinogens, pollution, and long-term infections.17 In addition to the avoidance of tobacco, the 2018 WCRF/AICR recommendations for cancer prevention focus on evidence-based modifiable lifestyle factors, including healthy weight, physical activity, and consuming a diet rich in whole grains, vegetables, fruits, and beans. Recommendations discourage using supplements for cancer prevention and state to limit consumption of fast and other processed foods high in fat, starches, added sugars, red and processed meats, sugar-sweetened drinks, and alcohol. Finally, mothers are recommended to breastfeed their babies if possible, as breastfeeding has been shown to protect against cancer. Further,18 those diagnosed with cancer are encouraged to follow the recommendations above.17
Greater adherence to the 2007 WCRF/AICR recommendations is associated with lower risk of total cancer as well as of breast and colorectal.9 For cervical cancer, the best form of prevention is HPV vaccination. Regular testing can also identify and treat pre-cancerous changes to prevent the most common form of this cancer from developing.19 According to both the Mayo Clinic20 and American Cancer Society,21 there is no known way to prevent testicular cancer13,21,22 due to the nonmodifiable risk factors mentioned above, though the following factors can add risk: age, cryptorchidism, family and personal histories, race, and HIV.
Reproductive Cancer Prevalence, Incidence, and Disparities
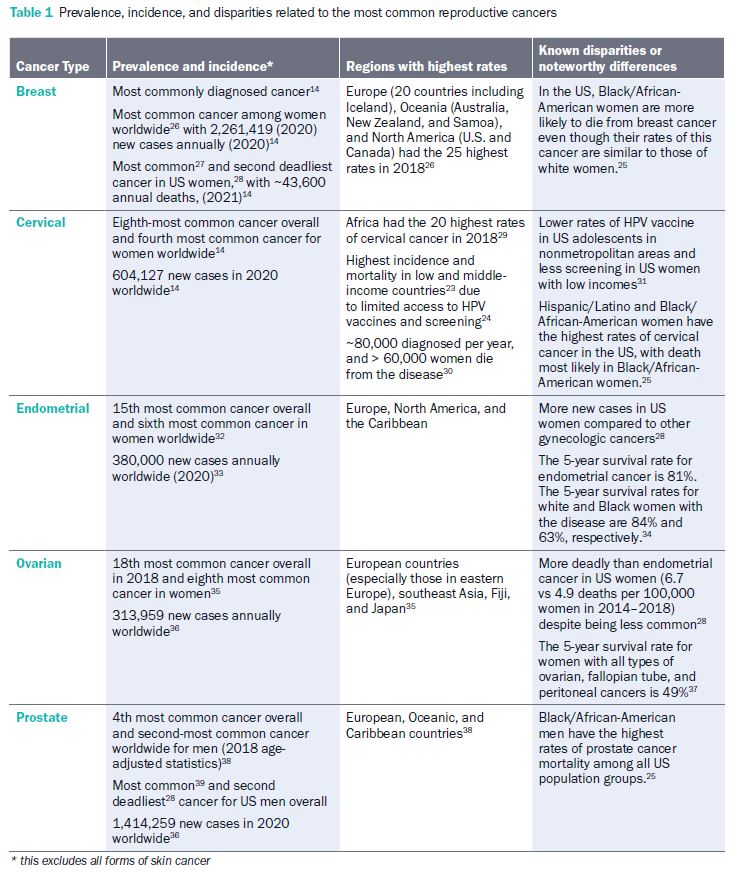
Reproductive cancers are more common in developed nations and regions defined by a Western lifestyle (Europe, North America, the Caribbean, and Oceania). Although incidence in high-income countries is greater, low- and middle-income countries have higher mortality rates from these cancers due to inadequate access to early detection from screenings and treatment.23,24 Within the US, disparities in the prevalence and mortality rates of reproductive cancers can be attributed to geography and race/ethnicity.25 The prevalence, incidence, and known disparities of common reproductive cancers are outlined in the table below.
Testicular cancer is relatively rare compared to other cancers, but it is the most common cancer among American males between 15 and 35 years old.13,16 Penile cancer which is highly HPV-related (>60%)40 is another rare cancer in North America and Europe,41 yet this cancer comprises 20% of cancers in African, Asian, and South American men.42
Dietary Risk Factors for Cancer
A poor diet alone may not cause cancer; however, some specific food items, food groups, and dietary patterns are known risk factors. Included among the known and probable human carcinogens identified by the International Agency for Research on Cancer and the US National Toxicology Program are alcoholic beverages, processed meat, and Chinese-style salted fish . Probable carcinogens include red meat and very hot beverages (above 65 degrees Celsius). In addition, epidemiological studies suggest that diets rich in animal foods (particularly with high amounts of saturated fat like fatty meats and dairy) and diets high in processed/refined foods may be associated with a higher risk of several cancers, including cancers of the breast and prostate.
Evidence from specific analyses and systematic reviews is provided below. Several studies have assessed associations between individual foods or food groups and reproductive cancers. A 2021 systematic review and dose-response meta-analysis included 75 studies assessing the association between breast cancer risk and various food groups, including red meat, processed meat, fish, poultry, egg, vegetables, fruit, dairy products (overall, milk, yogurt, and cheese), grains/cereals, nuts, legumes, soy, and sugar-sweetened beverages.43 From among these, higher intakes of red and processed meat and milk above 450 grams per day increased breast cancer risk.
A 2019 systematic review and meta-analysis also reported evidence with low to very low certainty that reducing processed meat consumption by three servings per week was associated with small decreases in prostate cancer mortality and incidence of breast cancer.44 Further, a 2014 systematic review of 46 studies assessing associations between nutrients, foods, or food groups and advanced prostate cancer risk found consistent evidence that diets habitually high in saturated fat, well-done meats, and calcium increased the risk of advanced prostate cancer.45
Studies have also explored associations between overall dietary patterns and reproductive cancers. Though conclusions are limited by potential recall bias, a 2018 review of 17 case-control studies that examined associations between dietary patterns and risk of breast canscer4 found that the unhealthy dietary patterns most associated with higher breast cancer risk consistently included saturated fat and red and processed meats. Some also included sugar- sweetened beverages, candy, refined grains, and fried foods . Compared to many other populations, Asians tend to consume more plant-sourced foods and fewer animal proteins, and they also have relatively low rates of breast cancer.
A 2007 study exploring dietary patterns and breast cancer incidence in Shanghai found that postmenopausal Chinese women following a “Western” dietary pattern high in shrimp, chicken, beef, pork, candy, and desserts had significantly higher odds of breast cancer than those following a more traditional dietary pattern centered around tofu, cauliflower, beans, bean sprouts, and green leafy vegetables.47 Correspondingly, dietary patterns high in processed meat and fatty dairy products are conducive to the development of prostate cancer through a variety of mechanisms, further discussed below.48
Benefits of Plant-Based Diets for Reproductive Cancers
Diets high in vegetables and fiber (fiber only comes from plant-food sources) are associated with a lower incidence of many forms of cancer, including the two most common reproductive cancers—breast and prostate. Overall healthy dietary patterns rich in whole grains, vegetables, fruit, and beans are recommended by the WCRF/AICR to prevent and reduce the risk of developing certain cancers49 as the 2018 systematic review mentioned above found: healthy dietary patterns protective against breast cancer consistently included vegetables, while some also included fruits, legumes, lean protein (fish, lean meat, low-fat dairy) and whole grains.46 Specific dietary patterns that generally follow the WCRF/AICR recommendations include the following:
- Mediterranean-style diet with high consumption of cereals, fruit, vegetables, legumes, fish; high monounsaturated/saturated fatty acids (MUFA/SFA) ratio; low consumption of dairy Mediterranean-style diet with high consumption of cereals, fruit, vegetables, legumes, fish; high monounsaturated/saturated fatty acids (MUFA/SFA) ratio; low consumption of dairy
- Prudent diet consisting of fruits, vegetables, whole grains, legumes, nuts, fish, and low-fat dairy products rather than refined or processed foods, red meats, high concentrated sweets, eggs, and butter51
- Dietary Approaches to Stop Hypertension (DASH) diet, rich in vegetables, fruits, and whole grains and includes fat-free or low-fat dairy products, fish, poultry, beans, and nuts while limiting foods high in saturated fat, such as fatty meats and full fat dairy products52
- Vegetarian diets characterized by an avoidance of meat and fish but may include dairy only (lacto-vegetarian) or dairy and eggs (lacto-ovovegetarian)53
- Vegan diets (strict vegetarian) that center on whole plant foods, characterized by an avoidance of all animal-sourced foods
- Whole food plant-based (WFPB) diet focused on natural, whole, unrefined, or minimally refined plant food ingredients and excludes animal
ingredients such as meat, milk, and eggs.54
Several studies support the use of these and similar dietary patterns to help reduce risk or improve prognoses related to reproductive cancers. In a cohort study of women from Northern Italy with breast cancer, those who adhered more strongly to a Mediterranean-style diet showed significantly better 15-year survival (63.1% survival) compared to those with low adherence (53.6%).50 Among women in the study over age 55 at diagnosis, the risk of breast cancer mortality was significantly lower for those with high versus low adherence to the Mediterranean diet. In India, where lifelong vegetarian diets are widely practiced, a 2018 study found that Indian women who followed a long-term lacto-ovo-vegetarian diet had lower odds of breast cancer than nonvegetarians and those vegetarians who avoided eggs.53 A 2002 study on Indian women who migrated to England found that lifelong vegetarians showed lower odds of breast cancer with higher intakes of vegetables, pulses (e.g., lentils), and fiber.55 Comparatively, in a 2018 cross-sectional study, odds of HPV infection, a potential cause of cervical cancer and tumors, were found to be related to dietary patterns.56 Here, women following a Western dietary pattern had higher odds of high-risk HPV infection, and women on a prudent diet had lower odds of high grade
cervical intraepithelial neoplasia than those not following these diets.
A recent eight-year prospective cohort study assessed dietary patterns associated with site specific cancers and found that prostate cancer risk was reduced in men following a prudent diet. As
adherence increased, prostate cancer risk decreased significantly.57 Those with the strongest adherence to this dietary pattern characterized by a high intake of grains, vegetables, and fruits showed a significantly reduced risk of prostate cancer compared to those who adhered least strongly.57 Epidemiological evidence linking diet to testicular cancer has shown inconsistent conclusions.
Results of some studies have shown an increased risk of testicular cancer with higher consumption of milk, cheese, and dietary fat, while other studies found no association.58
Mechanisms
A variety of biological mechanisms that increase or decrease cancer risk have been identified, and many though not all, are related to body composition, as described below.
Excess Weight and Obesity
Perhaps the strongest evidence linking diet to cancer is the effect of diet on excess weight and obesity, which are known risk factors for many cancers, including breast and endometrial. According to the National Cancer Institute, obesity may increase the risk of reproductive cancers, as described further here.59 Obesity often accompanies low-grade inflammation, which can cause DNA damage over time and, subsequently, lead to cancer.
In the case of female reproductive cancers, increased fat tissue results in excess amounts of estrogen, which are linked to cancers of the breast, endometrium, and ovaries. Obesity is also associated with increased blood insulin levels and insulin-like growth factor 1 (IGF-1), which can promote prostate and endometrial cancers, among others. Fat cells also produce hormones that can stimulate or inhibit cell growth, such that increases in body fat are associated with cell proliferation, while people with normal weight tend to produce more hormones with antiproliferative effects . In addition to hormones, fat cells also affect other cell growth regulators (e .g ., mammalian target of rapamycin, or mTOR, and AMP-activated protein kinase). Finally, obesity can alter breast tissue makeup, immune response, and oxidative stress, among other possible mechanisms.59
Evidence from the third expert report of the WCRF/ AICR revealed an increased risk of weight gain, overweight, or obesity with consumption of sugar- sweetened drinks and a probable increased risk with a Western-style diet and fast foods.60,61 A probable decreased risk of excess weight was found with dietary fiber consumption and a Mediterranean- type dietary pattern. Plant-based diets offer many advantages for healthy weight loss, in achieving a normal weight, and maintaining it.
Inflammation
Greater adherence to the 2007 WCRF/AICR recommendations was found to be associated with lower levels of biomarkers indicating oxidative stress and inflammation in premenopausal women.62 Another systematic review of 12 case-control studies found a positive association between an elevated inflammatory capacity of the diet as measured by the Dietary Inflammatory Index (DII) score and a higher risk of gynecological cancers among obese patients, particularly ovarian and endometrial. In contrast, components found in plant-based diets can reduce inflammation, including flavonoids, isoflavones, and other phytochemicals, as well as omega 3 fatty acids (particularly found in walnuts along with accompanying polyphenols, vitamin A, and other antioxidants), have been shown to reduce incidence of cancer from chronic inflammation effectively.63–67 These plant nutrients appear to suppress carcinogenesis through multiple pathways, including the ability to decrease or suppress activation of the protein pathway involved with cytokine production and activation of the NFκB transcription factor that may be a key link between inflammation and carcinogenesis.68
Insulin-like Growth Factor (IGF-1)
IGF-1 is a type of growth factor and cytokine69 that stimulates the growth of many cells in the body. Elevated blood levels of IGF-1 may increase risk of cancer. The predominance of plant-based diets in Asian countries appears to account for lower rates of some cancers and may be explained by lower circulating levels of total IGF-I and higher levels of IGFBP-1 and IGFBP-2 .70 Vegan men had 9% lower serum IGF-1 concentration compared with meat- eaters in one study71 and 13% lower levels among women who adopt a vegan diet in another.72 These concentrations suggest that the lower protein intake in the vegan diet may reduce serum IGF-I and increase serum IGFBP-1 and IGFBP-2 levels.72
Reactive Oxygen Species and Antioxidants
Elevated rates of reactive oxygen species (ROS) that promote tumor development and progression have been detected in almost all cancers. In part, ROS comprises free radical oxygen intermediates, which can cause damage to cells and tissues due to their instability from unpaired electrons.73 To stabilize these free radicals, tumor cells express increased levels of antioxidant proteins suggesting a delicate balance of intracellular ROS levels in cancer cell functionality.74 Antioxidants are naturally occurring compounds in plant foods that act as free radical scavengers and reducing agents, among other functions in the body,75 thus preventing some of the free radical damage known to be implicated in cancer development. Plant-prominent diets contain lower levels of ROS and high levels of antioxidants, whereas Western-style diets contain high levels of ROS and low levels of antioxidants.76 Dietary nutrients, including folate, carotenoids, and vitamin C, rich in vegetables and fruits, are significantly associated with reduced overall mortality (range 33–50%) after breast cancer diagnosis.77
Total Protein and Animal Protein Consumption
Protein consumption has been demonstrated to affect cancer promotion in animal models, with consumption levels predicting risk profiles in humans.78 In rat model experiments, alternate levels of the dairy protein casein fed to rats successfully turned on preneoplastic foci growth using a high- protein diet (20% calories coming from the protein) and then turned off the growth with a low-protein diet (5% casein). This suggests that low-protein diets inhibit lesion development, whereas high- protein diets encourage it.
The carcinogen-activating CYP27A1 enzyme can be highly responsive to increases in casein.79 Results of these animal models are supported by the comprehensive ecological study, the China–Cornell–Oxford Project conducted in 1983–1984, which found varying mortality rates for a wide variety of cancers and other chronic diseases throughout rural China,80 with such associations confirmed by more recent work.81 At that time, the breast cancer rate in China was positively associated with dietary fat intake, plasma cholesterol, and circulating estrogen activity.82,83 This relationship is further supported for overall cancer mortality when examining cancer incidence among individuals 50–65 years, with a 75% overall mortality increase and 4-fold increase in cancer death over the next 18 years.84 Associations were attenuated or abolished if the proteins were from plant foods.84
A Selection of Key Studies: Plant-Based Diets and Reproductive Cancers
Much research has examined the effects of plant-based diets on reproductive cancers, and especially breast cancer . Data from 10 studies with the most rigorous designs from our literature search are presented in Appendix Table 1 below. Of these studies, five were systematic reviews, meta-analyses, or both. Two studies were randomized controlled trials (RCT), and three were observational cohort studies. Four studies examined the relationship between plant-based diets and overall cancer risk,132–135 five studies examined breast cancer risk,133,136–140 two studies examined endometrial and ovarian cancer risk,141 and three studies examined prostate cancer risk.136,139,142 We found no studies examining the relationship between a plant-based diet and testicular cancer.
Of studies examining overall cancer risk, a posteriori derived (observational) plant-based dietary patterns were associated with a reduced risk of overall cancer incidence. An earlier study found that vegan and vegetarian diets were associated with a reduced risk of all-cause mortality and mortality from cancer. However, our analyses found some risk of publication bias in the reviewed articles.135
When examining breast cancer risk, one study found no reduced risk of breast cancer associated with vegan or vegetarian diets.136 However, one study, the California Teacher’s Study examining the relationship between a posteriori derived dietary patterns and breast cancer incidence, found that individuals who adhered most strongly to a plant-based diet had a reduced risk of breast cancer incidence compared to those who were nonadherent.137
An examination of the Adventist Health Study-2 found possible but unsubstantiated links between vegan and vegetarian diets and reduced risk of breast cancer.138 One study examining the relationship between diet and cancer outcomes post-diagnosis found that high intakes of saturated- and trans-fatty acids were associated with greater risk of all-cause mortality and non-breast-cancer mortality, and high protein consumption was associated with reduced risk of breast cancer recurrence and mortality from cancer. In addition, soy intake was associated with reduced breast cancer recurrence in this study.139 Another study found a reduced risk of breast cancer with higher serum carotenoid concentrations; however, participants assigned to a high-carotenoid diet and the control diet showed no difference in cancer risk.140
Finally, when examining prostate cancer, one study found no association between vegan and vegetarian diets and risk of prostate cancer, though a protective effect for overall cancer incidence was observed in cohort studies, and no increased risk from plant- based diets was observed.136 Another study found increased risk of cancer-specific mortality in those who consumed whole milk and chicken with the skin on, but not in red and processed meat. That same study found reduced cancer-specific mortality with high consumption of cruciferous vegetables and mixed associations with tomato products.139
One RCT found reduced need for traditional prostate cancer treatments like radical prostatectomy and radiotherapy with a lifestyle intervention including a low-fat diet, stress reduction, and increased exercise.142 Another randomized controlled trial by Ornish et al. confirmed these findings, showing a decrease in PSA and other factors, demonstrating a slowing of prostate cancer progression with a plant-based diet and lifestyle intervention.115 These randomized controlled trials suggest that wholistic lifestyle changes, including the adoption of a plant-based diet, would offer benefits and protection if incorporated into the standards of care.
Common Questions and Concerns
Are plant-based diets safe for cancer patients?
Yes, in fact, the American Cancer Society and American Institute for Cancer Research encourage the consumption of plant-based diets,17,49 as they are associated with lower overall risk134,143 and contain cancer-fighting phytochemicals and fiber.17 They recommend avoidance of processed meats, red meat, and added sugars which are associated with cancer risk.144,145 For those in treatment, optimal nutrition provides phytochemicals to support healing and recovery and avoid recurrence.115,146 Foods that provide these nutrients include vegetables, whole grains, legumes, and fruits. These foods can control inflammation, dampen the growth of abnormal pre-cancerous cells, and help the body function as best as possible. It is important to work with practitioners to avoid any foods that may interact with chemotherapy which may trigger adverse reactions from food intolerance.17
Do plant-based diets provide enough protein for cancer patients?
Yes. Legumes are a rich source of protein, dietary fiber, iron, zinc, folate, and potassium and are low in saturated fat, making them a healthier option than meat and dairy.17 Consumption of soy products is associated with lower risk of recurrence and higher survival rates among breast cancer patients.147,148 Including beans, whole grains, nuts, and seeds in the daily diet should provide more than enough protein for most patients,149 and working with a knowledgeable dietitian can help in planning a health-promoting diet with adequate protein for patients.
Will eating a plant-based diet cause weight loss in cancer patients?
Weight loss in cancer patients is not uncommon, particularly during chemotherapy or radiation treatments.150 For those with overweight or obesity, a plant-based diet will likely lead to weight loss and improved weight maintenance,17 which is associated with lower risk of reproductive and gastrointestinal cancers.17 But for those who need to build or maintain weight and muscle mass, this dietary pattern can provide the necessary protein to fulfill requirements as long as enough calories from whole foods are consumed.151 Concentrating on higher fat foods containing higher protein levels can help, particularly nuts, seeds, nut butters, and tofu.17,152 Eating throughout the day instead of a set three meals may allow the consumption of more calories throughout treatment.153 Whole food, plant-based enteral formulas may help when eating is difficult or with nausea.151,154
How can patients be encouraged to eat plant- based foods?
Patients trust their physicians for wellness advice and recommendations more than any other person.155 Practitioners can provide steps towards dietary improvement or therapy based on their readiness for change, starting with simple suggestions and avoiding overwhelming the patient with a big dietary overhaul.155 They can offer resources like those provided by ACLM at lifestylemedicine.org, including meal plans, shopping lists, and nutritional information. Emphasizing the many benefits of healthy plant-predominant eating, including better health outcomes in general, leading to lower healthcare costs, can motivate patients. Lastly, health professionals who model good lifestyle behavior will inspire their patients to make healthy food decisions.156
Do plant-based diets have any adverse interactions with chemotherapy or radiation treatments?
Plant-based diets may pose certain challenges during cancer treatment, but they can be resolved through planning, as it may be harder to maintain body mass and keep from losing too much weight during cancer treatment on a plant-based diet. Patients may benefit from a personal weight-management plan or suggestions from an oncology dietitian. Malnutrition can impair the body’s response to treatment, and thus, the National Cancer Institute recommends a diet assessment early on and monitoring at all phases of recovery.150 Citrus fruits, pineapple, and tomatoes may irritate the mouth during chemotherapy, particularly if mouth sores are present.153
Digestive issues may demand adjustment of fibrous foods. For constipation, high-fiber foods like peas and whole grains may help, and for loose bowels, high sodium and potassium foods may help, including broth, bananas, peaches, or apricot nectars; also bland, low-fiber foods such as rice noodles, boiled potatoes, farina, white bread, canned fruits or well- cooked vegetables may be well-tolerated.150
Download the full 181 page Benefits of Plant-Based Nutrition White Paper for access to all references, key studies and more.
Promising Results: Plant-Based Diets as Part of Medical Treatment
Further research on the effects of plant-based diets as part of cancer treatment is merited. The following encouraging results from the Prostate Cancer Lifestyle Trial (PCLT)142 indicate that prescribing a plant-based diet as part of care may offer meaningful benefits for patient. The Prostate Cancer Lifestyle Trial (PCLT)142 found that patients with early-stage prostate cancer choosing active surveillance might be able to avoid or delay costly and invasive conventional treatment for at least two years by making changes in their diet and lifestyle (N=93 men; mean age 66 ± 8 years with biopsy-proven prostate cancer; Gleason score <7, PSA 4–10 ng/mL). Intervention patients were prescribed a low-fat, plant-based diet. After two years of follow-up, a total of 27% of control patients and only 5% of intervention patients had been treated with conventional prostate cancer treatment (radical prostatectomy, radiotherapy, or androgen deprivation, P < .05). The experimental patients also had greater improvements in cardiovascular health parameters than did control patients. These findings are noteworthy because avoiding the need for conventional treatment even after cancer diagnosis can translate to improved quality of life and reduced healthcare costs.
Conclusion
Current research indicates that lifestyle factors play a pivotal role in cancer development and health promotion . In particular, whole food, predominantly plant-based diets offer a variety of benefits for cancer prevention, and their use as part of cancer care may aid conventional treatment. Focusing on a healthy, plant- predominant diet can be a key component of cancer treatment to support health and optimal outcomes.
Download the full 181 page Benefits of Plant-Based Nutrition White Paper for access to all references, key studies and more.
CONTINUE READING IN THIS SERIES
- The Benefits of Plant-Based Nutrition
- The Benefits of Plant-Based Nutrition: Diet Quality
- The Benefits of Plant-Based Nutrition: Obesity & Weight Management
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Type 2 Diabetes
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Cardiovascular Disease
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Chronic Kidney Disease
- The Benefits of Plant-Based Nutrition: for Enteral Nutrition
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Reproductive Cancers
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Autoimmune Disease
- The Benefits of Plant-Based Nutrition: Longevity and Quality of Life
Acknowledgement
This review was made possible in part due to a generous donation from Kate Farms. For more information on Kate Farms, please visit their website here: www.katefarms.com