The Benefits of Plant-Based Nutrition: Treatment and Prevention of Chronic Kidney Disease
Whole food, plant-based diets offer two advantages for prevention and treatment of CKD. First, higher consumption of plant foods are protective against the disease; second, lower consumption of animal and higher protein foods reduce renal burden.
Abstract
Dietary patterns focusing on whole plant-based foods may be pivotal in managing chronic kidney disease (CKD). Predominantly plant-based diets may delay progression and help to control common chronic conditions that are often associated with CKD, including type 2 diabetes, cardiovascular disease, hypertension, obesity, and kidney stones, improving multiple comorbidities simultaneously.1 Provided that potassium levels are monitored, plant-based diets pose minimal to no
risk for CKD patients and may delay or avoid the need for dialysis.2–4
Consuming plant protein over animal protein treats and prevents CKD,5 and the fiber in plant foods allows for a shift away from the production of uremic toxins and other nitrogenous wastes. The lower protein level of a plant-based diet has favorable effects on secondary hyperparathyroidism,6 peripheral insulin resistance,7 hyperlipidemia,8 hypertension, and acid-base disorders.9 Plant anions may mitigate metabolic acidosis to slow CKD progression. Plant phosphorus has a bioavailability of less than 50% as compared to animal phosphorus, and phosphorous is identified as a burden on the kidneys and may worsen renal osteodystrophy and hyperparathyroidism.10 Both the reduction of phosphate in the diet, as well as its source (animal- versus plant-derived) appear to be important.5 For those with CKD, goals can center on slowing the progression of kidney failure, minimizing uremic toxicity, diminishing proteinuria, and lowering the risk of complications, including cardiovascular disease, bone disease, and blood pressure control.11 A plant-based diet naturally lower in protein has been shown to help accomplish all of these treatment goals.5
Key Points for Practitioners
- Whole food, plant-based diets offer two advantages for prevention and treatment of CKD. First, higher consumption of plant foods are protective against the disease; second, lower consumption of animal and higher protein foods reduce renal burden.25
- Animal foods do not contain fiber. Fiber aids in creating and maintaining a healthy microbiome to address toxins, as well as producing anti-inflammatory compounds and reducing the production of uremic toxins. Fiber also controls potassium absorption to avoid hyperkalemia, and those who need to restrict potassium content can focus on low potassium plant foods, such as such as apples, berries, cabbage cauliflower, eggplant, and yellow squash.2,26–28
- Plant-based diets are the key to controlling acid load to keep metabolic acidosis in check and thus slow progression of kidney disease.25,26
- Plant-based diets, rich in fruits, vegetables, dietary fiber, and potassium, are associated with lower risk of kidney stone formation versus animal-based diets.27
- Unrefined plant food intake lowers risk of hyperphosphatemia, as phosphorous is bound to plant phytates.20
- Marked improvements in all markers of CKD (albuminuria, metabolic acidosis, hyperphosphatemia, hypertension, glycemic control) have been documented in patients following a whole food, plant-based diet.28
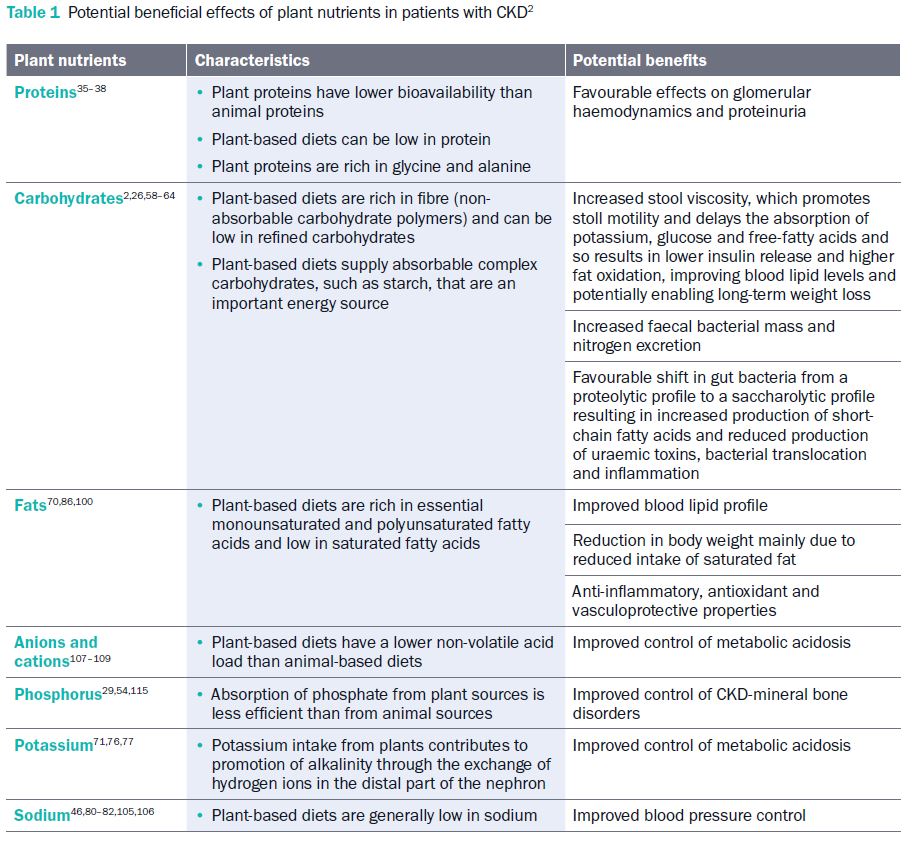
- Specific dietary components are associated with specific benefits for CKD (see Table 1).
- Adherence and satisfaction with plant-based diets among elderly patients appear to be equivalent to more conventional lower-protein diets.29
- Whole food, plant-based diets are associated with other health benefits such as cardiometabolic health, healthy weight, and longevity.1
- Existing evidence on plant-based diets and CKD can be communicated to patients to support their ability to make informed decisions about their diet and course of treatment.1
- If patients express interest in trying a whole food, plant-based diet of some kind, it is helpful to share ACLM patient-facing resources and tools for practical guidance on plant-based eating.
Chronic Kidney Disease in Context
Chronic Kidney Disease (CKD) describes the gradual loss of renal function: filtering wastes, toxins, and excess fluids from blood to be excreted in the urine.
Electrolytes and wastes accumulate until kidney function is significantly impaired, often with few symptoms in the early stages of the disease.12,13
As one of the top ten leading causes of premature death,14 CKD affects more than one in seven American adults (15%) or 37 million people. Most
(90%) individuals with CKD do not know that they have it.15 Diabetes and high blood pressure are common comorbidities and the leading causes
of end-stage renal disease (ESRD), which is also associated with increased all-cause mortality.16
Other risk factors include obesity, older age, glomerulonephritis (a disease that damages the kidney’s filtering units), inherited diseases such as polycystic kidney disease, malformations at birth, lupus or other immune diseases, and obstructions such as kidney stones or an enlarged prostate, as well as repeated urinary tract infections.17
Treatment of chronic renal failure can be challenging since individuals may not feel ill or present symptoms until advanced stages.18 Comorbidities may be
recognized and treated first without consideration of renal risk, and though recommendations to follow a healthy diet may be offered to keep CKD from worsening, there is much confusion over what constitutes a healthy diet, even among practitioners.
Low protein diets are recognized as beneficial, but adherence to conventional low protein dietary substitutes can be low due to palatability and cost. The Kidney Disease Outcomes Quality Initiative (KDOQI) nutrition guidelines were recently updated to “suggest that increased fruit and vegetable intake may decrease body weight, blood pressure, and net acid production” based on a grade 2C recommendation,19 which aligns with the tenets of lifestyle medicine.
Benefits of Plant-Based Diets for Chronic Kidney Disease
Focusing on plant-based foods to improve diet quality for CKD patients while reducing total animal-based foods has been shown to improve kidney function.2-4 These dietary improvements reduce the need for medications, reduce disease complications, decrease progression, and, thus, increase patient survival.2,20 Observational data demonstrate an association between red and processed meat and an increased risk for CKD. One cross-sectional study (N=5,316) found that those with the highest plant protein intake demonstrated a 30% lower risk for CKD compared to those with the lowest. Conversely, the highest quartile of animal protein intake had a 37% higher risk for CKD.21 In another study, a pattern of high intakes of whole grains, vegetables, fruits, and low-fat dairy foods was associated with a 20% lower urinary albumin-creatine ratio (the measure for protein loss in the urine indicating kidney malfunction).22
Whole food, plant-based diets have the dual advantages of supplying nutrients and antioxidants that support and potentially heal damaged kidneys and eliminate the processed and animal foods associated with greater risk for CKD.23,24 For patients with CKD, focusing on dietary quality instead of traditional recommendations that focus on the quantity of nutrients consumed could revolutionize treatment from simply lessening the damage to healing, with few risks.20
Chronic Kidney Disease and Dietary Mechanisms
Several underlying mechanisms play a role in kidney dysfunction and CKD progression. This includes a decreased glomerular filtration rate (GFR), used to measure kidney function, which may be due to elevated dietary acid load, as the retention of acid is associated with downstream effects of kidney function.30,31 Metabolic acidosis is a common complication of CKD resulting from the
inability of the kidneys to excrete the daily dietary acid load. Metabolic acidosis increases the risks of hypertension,32 heart failure,33 muscle wasting,34 bone loss, chronic inflammation, progression of renal failure, and death.35 High-protein diets may worsen kidney function in individuals with kidney disease from the body’s demand to eliminate the excess waste products of protein metabolism. High-protein diets are also associated with higher urinary calcium excretion, increasing risk for kidney stone formation.36 High-protein diets are associated with increased metabolic acidosis and oxidative stress, contributing to kidney damage.37 Further, these diets will likely limit the bioactive compounds, including isoflavones and fiber, that control glycemic load and protect the kidneys.38
With respect to mortality, one study found a decreased risk of all-cause mortality in end-stage renal disease patients with higher plant-based diet pattern scores.39 Two studies found benefits from low-protein, plant-based diets supplemented with ketoanalogues.6,40 Improvements in serum phosphate and calcium levels were also noted, along with a reduction in parathyroid hormone levels.40 Another study found a very low protein, vegan diet to be safe and effective in elderly patients with Stage 5 CKD in delaying the onset of dialysis.41
Protein Quality? Plant-Based vs. Animal Proteins
Some CKD patient guidelines emphasize protein from animal sources due to their “high value” to assure that essential amino acids are not limited, but this measurement is based on animal studies and considered outdated.42 Plant-based proteins contain all essential amino acids and offer the benefits of the fiber and isoflavones present.43 Dietary interventions can be particularly effective in controlling protein intake. For example, varying oral protein intake levels affect GFRs in subjects with healthy kidneys, and chronic excess protein consumption can inhibit function.44–46 This was demonstrated decades ago in a study that administered a vegetarian soy-based diet, low in both fat and protein for two months resulting in highly significant decreases in total serum cholesterol (28%). The soy diet had other benefits, such as lowering LDL-cholesterol, apolipoprotein B, and urinary protein excretion, all reversed upon discontinuation of the diet.47 No other treatment for kidney disease has been shown to lead to disease reversal by addressing the underlying development of disease.
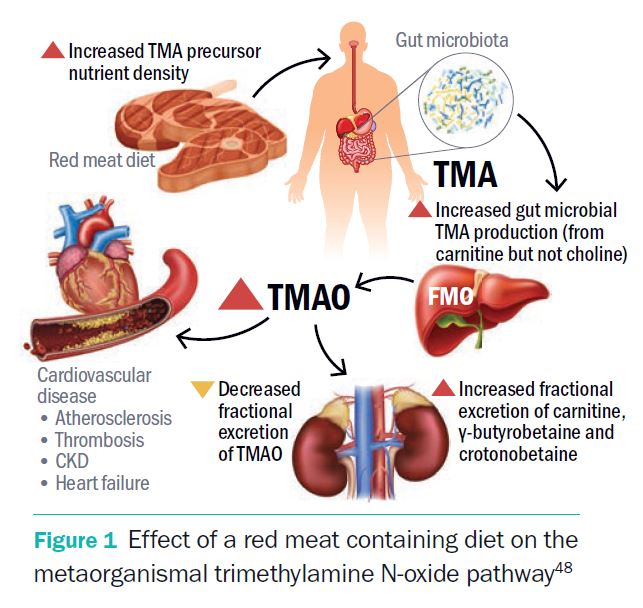
Higher risk from animal proteins is likely due to the acidic quality of meat, and the creation of more metabolites in the gut and their effective excretion, particularly trimethylamine N-oxide (TMAO). TMAO is the byproduct of the breakdown of the amino acid carnitine in meat associated with an increased risk of heart disease.48 High circulating levels of TMAO are linked with increased risk for chronic kidney disease and kidney fibrosis development. In addition, animal studies show that reducing TMAO results in improved CKD and cardiac hypertrophy.49 Research suggests that the kidney becomes less efficient at eliminating TMAO with increased red meat intake, and, quite remarkably, discontinuation of red meat reduces plasma TMAO within 4 weeks.48
The primary source of acid production in the body can be traced to diet. Acid in the diet comes primarily from protein which releases sulfuric acid when metabolized. The Western diet favoring animal protein made of sulfur-based amino acids promotes an acidic environment in the body.26,50 In contrast, plant foods are alkaline, which protects against dietary acid load. Plant-based proteins satisfy requirements for those with CKD and offer other inherent health benefits compared with animal-based proteins.16,31,36,47,51,52 Research suggests that in people with decreased kidney function, substituting animal foods from the diet with plant protein sources is associated with a lower CKD risk.24,53
Hyperphosphataemia
Hyperphosphataemia is a condition of excess phosphorus levels in the blood, commonly caused by kidney failure. As increasing amounts of phosphorus are absorbed from red meat, dairy, chicken, and fish, phosphorus is filtered through the kidney, and levels in the blood rise.54 Plant foods offer an advantage here because phosphorus is not as efficiently absorbed from plant sources compared to animal sources, thus decreasing the burden on the kidneys.29
Whole plant foods provide higher amounts of magnesium, an effective inhibitor of calcium oxalate growth (kidney stones),55 whereas a high calcium diet emphasizing dairy may inhibit magnesium absorption.56,57 Plant foods also provide antioxidants to combat free radical damage, as well as the optimal ratios of essential fatty acids,23,58 indicating that a diet full of whole plant foods offers protection against hyperphosphatemia, a concern for CKD patients.20
Toxins, the Microbiome, and Fiber, the Hidden Hero
Polysaccharides found in plant foods contain dietary fiber to decrease toxins and facilitate the excretion of nitrogen. Fiber increases fecal bacterial mass, as shown in a meta-analysis of 14 controlled trials.59 This non-digestible polymer is consistently associated with lower blood lipid levels, total cholesterol, and body weight, all of which lower stress on the kidneys.60,61 In observational studies, fiber was associated with a higher estimated glomerular filtration rate (eGFR), lower inflammation, and a lower CVD risk,62–64 though similar outcomes are not necessarily observed for isolated fiber supplements.65
Fiber intake increases intestinal motility as well as fecal excretion. It allows the gut microbiota to build numerous beneficial colonies of bacteria and reduce uremic toxin production. Despite evidence demonstrating the benefits of plant-based diets containing fiber, most CKD patients consume well below recommendations (25 g/day for women and 38 g/day for men66). Nutritional guidelines do not highlight the benefits of consuming foods with fiber, which include protecting the kidneys against dialysis.67–70 In addition, whole plant-food treatment can lower production of uremic toxins.25
Gut microbiota breaks down and ferments animal protein, which produces toxins normally cleared by the kidneys. Excessive animal food in the diet of CKD patients leads to alteration of the colonic environment in microbial dysbiosis and disturbances in the intestinal mucosa barrier. This state enables bacteria and endotoxins to slip through the intestinal barrier, which in turn stimulates monocytes and leads to increased synthesis of inflammatory cytokines.2
Hyperkalemia
Although there is a concern about hyperkalemia in CKD patients, recent case studies indicate that lack of fiber from whole foods may be the ameliorating factor. Because fiber promotes stool
quantity and frequency, it facilitates the excretion of potassium.60,71,72 Restricting plant foods for these patients deprives them of their benefits.73 Fruits and vegetables are naturally rich in potassium and readily absorbed by the proximal intestine, but absorption may be influenced by alkaline load and the fiber available to facilitate deposition and decrease transit time.74
Feeding trials in healthy people suggest that potassium recovery from animal-based diets is about 80% and 50–60% from plant-based diets.75,76 Hyperkalaemia is a concern because high potassium can rapidly cause arrhythmias without symptoms. Caution around potassium intake and monitoring is advisable. The lower availability of plant potassium may be advantageous to CKD patients without precipitating hyperkalemia;77 however, close monitoring of all patients’ potassium levels as they transition to a whole food, plant-based diet is essential to facilitate any medication adjustments that may be needed by the practitioner.
Kidney Stones
Though the oxalate content of plant foods has been a concern, observational studies indicate that vegetarians have a lower risk for kidney stones,78,79 likely due to higher alkali and water levels and the reduced sodium within plant foods.80–82 The inconsistency could also relate to the microbiome and the recently discovered role of Oxalobacter formigenes and other bacteria that require oxalate for survival which may reduce the amount of oxalate available for absorption and, ultimately, excretion in urine,51,83 though more research in this area is needed.
Filtration
Animal-based protein induces hyperfiltration,26,84–86 which temporarily overworks the kidneys, while an equivalent amount of plant protein does not induce the same stress. One study found that an animal protein-based diet led to hyperfiltration with increased GFR versus a plant-based protein diet in nonproteinuric patients with type I diabetes.86,87 Conversely, one study found an increased risk of albuminuria with Western dietary patterns derived a posteriori. In the same analysis, the authors found a decreased risk of microalbuminuria in DASH designated
dietary patterns.72 Hyperfiltration over the long-term is linked with irreversible damage of nephrons and development of progressive kidney disease as seen in diseases such as diabetes.88
Common Questions and Concerns
The need for low-protein, low potassium diets may indicate that plant-based diets are not ideal for patients with compromised kidney function.
Though plant foods generally contain more potassium than animal foods, the accompanying fiber decreases potassium absorption and helps to avoid hyperkalemia by facilitating the excretion of potassium.60,71,72 Fruits and vegetables are naturally rich in potassium which is readily absorbable by the proximal intestine. However, absorption may be influenced by alkaline load. Since the metabolic breakdown of proteins increases acidity, meat and cheese have the highest potential for renal acid load, whereas fruits and vegetables have the lowest. Also, dietary recall may underestimate potassium consumption by failing to account for the cooking loss. Soaking, freezing, or boiling leads to a 60–90% potassium loss of several raw foods and introduces inaccuracy by not accounting for this differential bioavailability.89,90 Sauces and juices lack fiber, which uniquely increases potassium consumption compared to whole food form. Plant foods with low potassium content, such as apples, berries, cabbage cauliflower, eggplant, and squash, are a good choice for those who need to restrict potassium. Other low-potassium plant foods include
bread, noodles, and rice.91,92
What is the proper diet for those on dialysis?
There is a paucity of evidence evaluating the potential benefits of plant-based diets in patients undergoing dialysis. However, one recent study revealed that function of daily activities in hemodialysis patients on vegetarian diets was similar to that of non-vegetarians.93 Two studies showed that soy consumption reduced inflammatory markers and lipoprotein (a) levels.94,95 Though nutritional indicators such as BMI or muscle mass might be lower among dialysis patients, dialysis adequacy can be maintained with a plant-based diet, which has the advantage of higher nutritional value than traditional dietary recommendations.93
Traditionally, patients on dialysis are discouraged from adopting plant-based diets mainly due to two perceived risks: inadequate protein intake and hyperkalemia, yet general population studies show that the risk of nutritional deficiencies from plant-based diets is low. Even strict vegans meet the minimum requirements for protein.96,98 Further, patients on dialysis on plant-based diets have also been reported to attain adequate protein intake (1.1–1.25 g/kg/day) without signs of undernutrition.93,99 Though research of patients on dialysis adhering to plant-based diets is limited, the linoleic acid (omega-6 polyunsaturated fatty acid) level as a proportion of total plasma fatty acids was demonstrated to be inversely associated with markers of inflammation
and risk of death.100 Oils, meats, and eggs are rich sources of linoleic acid.101 Low-fiber intake has also been associated with higher concentrations of inflammatory biomarkers.102–104 All dialysis patients should supplement with B vitamins as these are water-soluble and readily lost with dialysis.
How concerning is the high phosphorous level in plant foods for those with compromised kidney function, and why?
Though phosphorous is in plant foods, it is not absorbed efficiently. Animal protein is the primary source of bioavailable phosphorus.26 Phosphorous in plant foods is primarily bound to phytate, which is poorly absorbed since humans lack the enzyme phytase to break it down. Thus, a plant-based diet may be beneficial in reducing the phosphorus load on the body and improving vascularization.26
The benefit and workload comparison of the standard low-protein diet (such as the National Kidney Foundation’s diet) is often recommended. Is it a plant-based diet?
The National Kidney Foundation states: “Eating more plant-based foods such as vegetables and grains in place of animal-based foods such as red meat may help prevent and slow the progression of chronic kidney disease, type 2 diabetes, high blood pressure, and heart disease.”105 On their website they recommend the DASH Diet (Dietary Approaches to Stop hypertension) or a Plant-Based Diet.106 Plant-based diets reduce the renal load on the kidneys, from the accompanying fiber, from avoidance of excess protein, and a reduced acid load. The kidneys regulate acid-base homeostasis, and acid-load is primarily modulated by diet.2 A higher acid load accelerates kidney damage and eGFR decline, whereas an alkaline diet reverses these processes.107–109 Compared with animal-based diets, plant-based diets have a lower non-volatile acid load, as they are richer in organic anions than cations. Additionally, the increased fiber intake found in plant foods allows the gut microbiota to generate more short-chain fatty acids, which are alkali. The alkali state reduces the generation of uremic toxins, which also contributes to the alkaline state.110–114
Summary of Key Studies
A selection of more high-quality studies relevant to plant-based diets and CKD outcomes is displayed in Appendix Table 1. Multiple studies demonstrate favorable associations and clinical markers for CKD between plant-based diets, naturally low in protein. The risk of kidney stones from uric acid crystallization decreases with vegetarian diets,52 as does fibroblast growth factor-23 (FGF23). Both phosphorous excretion and accumulation show improvement,115 as do glomerular filtration rate (eGFR), renal plasma flow (RPF),86 and albuminuria; thus, mortality rates are better as well, as summarized in Table 1, below.39,41,65,72,116 In the one study examining uric acid crystallization, the authors found that the risk of crystallization was reduced in those randomized to a vegetable protein diet (VPD).52 Another study that examined fibro-blast growth factor-23 (FGF23) plasma levels demonstrated that a vegetarian dietary intervention decreased FGF23 levels. FGF23 is responsible for maintaining phosphorous homeostasis. A decrease in FGF23 indicated a decreased phosphorous load due to reduced absorption in vegetarian diets.115
Such findings are not new to the literature. A 1995 study on eGFR found that a vegetable protein dietary intervention in nonproteinuric type I diabetes patients led to decreased eGFR and renal blood flow, suggesting decreased renal load is associated with plant protein.86 Considering that diabetic kidney disease is the most prevalent form of CKD and the leading cause of end-stage kidney disease, plant-based dietary interventions may be capable of largely reducing mortality rates.14 In fact, a 2011 prospective cohort analysis of the Nurses’ Health Study data found an increased risk of albuminuria from Western dietary patterns along with the decreased risk of microalbuminuria using the plant predominant DASH dietary patterns.72 Though fiber has been demonstrated to be a critical factor in renal outcome by controlling waste products left to the kidneys to filter,117 one study found no difference in the eGFR and albuminuria between randomized groups taking a soluble fiber supplement and those without supplementation.65 This may indicate that many of the benefits of fiber intake likely come from intact fiber found in whole plant food itself and not from isolated fiber in supplemental form.65
With respect to mortality, more than one study found a decreased risk of all-cause mortality in end-stage renal disease patients with higher plant-based diet pattern scores, as well as a significant association between plant-based diets and slower renal function decline.39,116 Another study saw improvements in serum phosphate and calcium levels while reducing parathyroid hormone levels on a plant-based diet supplemented with ketoanalogues.40 Finally, another found equivalent survival with a low-protein, plant-based diet intervention compared to dialysis treatment in senior CKD patients.41 As Table 1 describes, the literature indicates that plant foods with intact fiber have an irreplaceable role in overcoming CKD, its comorbidities, and the risk for mortality.
Download the full 181 page Benefits of Plant-Based Nutrition White Paper for access to all references, key studies and more.
Promising Results: Cases of Improved Longevity and Quality of Life
Though research on interventions that produce remission is still emerging, the following examples are promising and support the value of incorporating a dietary intervention even when other treatments are also used.
Reversal of CKD in an Elderly Man with Multiple Comorbidities
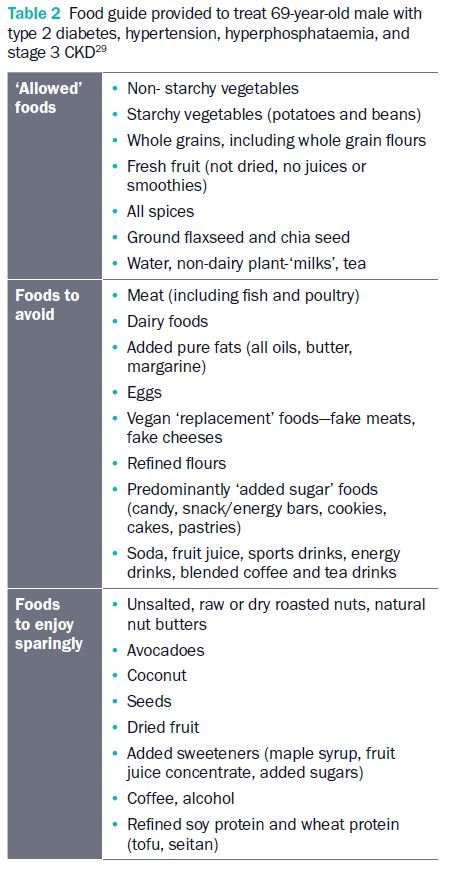
A recent case study demonstrates the ability of a strict whole food, plant-based diet to restore health for a 69-year-old male with type 2 diabetes, hypertension, and stage 3 CKD.29 His history included class 2 obesity, hypertension, hyperlipidemia, and type 2 diabetes, requiring approximately 210 total insulin units daily (140 units insulin glargine and ~20–25 units insulin lispro) and three meals daily. After comprehensive counseling, being provided a food guide, and switching to a whole food, plant-based diet without calorie or portion restriction or mandated exercise, the patient rapidly reduced his insulin requirements by >50% and subsequently experienced improvements in weight. He was taken off carvedilol, hydrochlorothiazide, amlodipine, and sitagliptin within the first two months due to blood pressure, blood glucose, and cholesterol improvements. His estimated eGFR increased from 45 to 74 mL/min after 4.5 months post-dietary transition. His pravastatin dose was cut in half, and microalbumin/creatinine ratio decreased from 414.3 to 26.8 mg/g. Phosphorus level returned to the normal range. See Table 2 for the food guide provided by his physician.29
Multiple Conditions Controlled by the Creeping Polypharmacy
This case details a 57-year-old woman with essential hypertension, obesity, type 2 diabetes, hyperlipidemia, and CKD, a set of comorbidities that is not uncommon in the US. She presented with a GFR between 31 and 35 mL/min conferring a kidney disease classification of G3bA3 (moderately to severely decreased renal function with severely increased albuminuria). Her conditions required multiple medications to control, and the need for polypharmacy continued to increase. This patient was motivated to include more whole grains, fruits, vegetables, and legumes into her diet and reduce her consumption of processed foods, refined grains, added sugars and salts, and animal products. After three months, her blood work showed improvement in metabolic acidosis, proteinuria, and hyperphosphatemia without an increase in serum potassium levels. She was not only able to avoid additional medications but reduced her existing medication burden, including calcium acetate (phosphorous binder), amlodipine (antihypertensive), and sodium bicarbonate (reduce metabolic acidosis). This patient’s dietary change directly resulted in improved kidney function, improved quality of life, and reduced risk of mortality.1
Appropriate Protein Consumption for the Elderly
A plant-based dietary approach with its high nutritional value and lower protein values may resolve issues of compliance with restrictive “traditional” low-protein diets in elderly patients
with kidney disease. Though protein restriction may retard the need for renal replacement therapy, high protein intake is believed to contribute to preserving nutritional status in elderly patients or in patients with high comorbidity. Mediating between conflicting requirements can be a challenge, but Fois et al. detail a feasibility study (N=131) in which all patients attained the goal of appropriate protein reduction intake for advanced kidney disease using a stepwise approach to a high-nutrient diet.118 The 131 patients [median age (range)= 74 (24–101)] had multiple comorbidities upon entering the study at an advanced kidney disease unit in Le Mans, France. Twenty-two (17%) chose to comply with a plant-based diet and showed improvements in Charlston Comorbidity Index (CCI) and eGFR. All patients attained the goal of protein reduction intake of at least 0.2 g/kg/day in ≥ 3 months of follow-up, and note that each decrease of at least 0.2 g/kg/ day of protein is associated with a reduction in the deterioration of kidney function. Good compliance was found in 74%, regardless of diets, indicating that treatment with low-protein, plant-based diets should not be a barrier to compliance. Even in a population with high comorbidity, a personalized approach to reduced protein intake is feasible, including with diabetic patients and in elderly individuals.118
Conclusion
Studies indicate that the benefits of plant-based diets can be applied to all populations to address kidney dysfunction, even in the elderly at advanced stages. Plant-based diets have been demonstrated to be safe and useful in preventing and treating all chronic diseases, including type 2 diabetes, obesity, hypertension, and hyperlipidemia, which are common comorbidities of CKD. The utility of plant-based diets for CKD has become increasingly apparent.1,119–121 The research discussed here has indicated a reduced risk of albuminuria, uric acid crystallization, stone formation, improved eGFR markers, and reduced acid and waste loads in individuals using lower-protein plant-based diets. Shifts towards plant-based proteins, reduced animal proteins, and reduced overall protein consumption show great promise for improving CKD outcomes, including halting renal function decline, reducing the need for dialysis, and ultimately saving lives.
Though plant protein consumption is consistently associated with reduced renal load, more evidence is needed to demonstrate the long-term benefits of plant-based diets on individuals with CKD or end-stage renal disease.2,65 Overall, existing evidence indicates that diets rich in fruits and vegetables can reduce the dietary acid load and offer an exciting approach to treating CKD by reducing kidney damage, slowing disease progression, and, most importantly, helping patients improve their quality of life.91
Download the full 181 page Benefits of Plant-Based Nutrition White Paper for access to all references, key studies and more.
CONTINUE READING IN THIS SERIES
- The Benefits of Plant-Based Nutrition
- The Benefits of Plant-Based Nutrition: Diet Quality
- The Benefits of Plant-Based Nutrition: Obesity & Weight Management
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Type 2 Diabetes
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Cardiovascular Disease
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Chronic Kidney Disease
- The Benefits of Plant-Based Nutrition: for Enteral Nutrition
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Reproductive Cancers
- The Benefits of Plant-Based Nutrition: Treatment and Prevention of Autoimmune Disease
- The Benefits of Plant-Based Nutrition: Longevity and Quality of Life
Acknowledgement
This review was made possible in part due to a generous donation from Kate Farms. For more information on Kate Farms please visit their website here. www.katefarms.com