Lifestyle medicine works. So why can’t physicians get paid to practice it?
What is missing is a model that allows clinicians to integrate lifestyle medicine into their practice, incentivize the most optimal health outcomes and make it financially sustainable. But solutions could be coming.
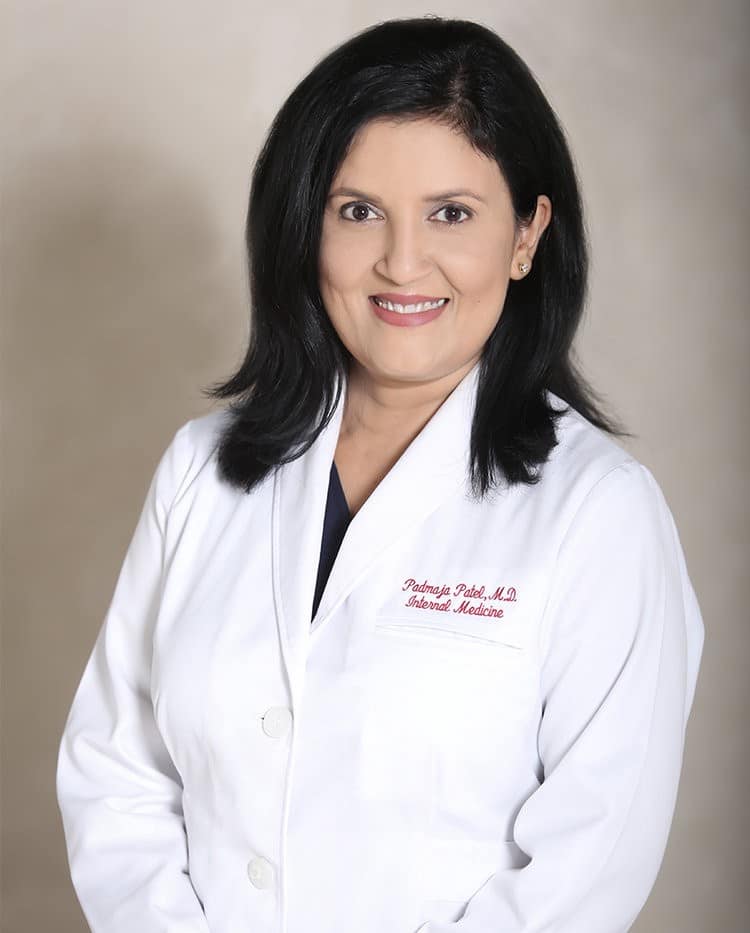
As a passionate advocate for lifestyle medicine, Padmaja Patel, MD, DipABLM, knows many clinicians committed to practicing the fast-growing field and dedicated to restoring their patients’ health through proven, evidence-based treatments.
But they struggle with financial unsustainability in a system geared more toward “sick care.”
The predominant U.S. fee-for-service health care reimbursement model rewards clinicians for how many procedures and services they perform, not for making their patients healthy again. In addition, quality measures tied to physician payment reward process such as prescribing a medication and assuring compliance and penalize successful outcomes such as restoring a patient’s health through nutritional and exercise lifestyle interventions instead.
In fact, in a survey of 1,286 physicians and other clinicians, 55 percent reported not receiving any reimbursement for lifestyle medicine practices, while 27 reported some reimbursement and only 18 percent were reimbursed for all their lifestyle medicine interventions, according to research published recently in the International Journal of Environmental Research and Public Health. This despite the majority of clinical guidelines for treatment and management of chronic disease recommending lifestyle changes as a first-line intervention.
Survey respondents described billing for lifestyle medicine as “prohibitive” and “no one knows how,” and lamented constraints on time available to properly educate patients during appointments, as well as time to develop materials and programs.
Dr. Patel, medical director of the Lifestyle Medicine Center at Midland Health, Midland, Texas, and a team of experts affiliated with the American College of Lifestyle Medicine (ACLM) want to change that. The Clinical Practice and Quality Committee, formed in fall 2021, is working to create a model that will allow clinicians to integrate lifestyle medicine into their practice and remain financially viable. To seed the project, Dr. Patel made a generous $10,000 personal gift and has challenged fellow like-minded clinicians to join her in trying to raise $100,000.
“We have done an excellent job proving that lifestyle medicine works and that the science supports lifestyle medicine as a first-line treatment for many chronic diseases,” Dr. Patel said. “It is even the first-option treatment recommended in most chronic disease clinical guidelines. What we have not yet done is to demonstrate to clinicians an effective model for integrating lifestyle medicine into their practice and make it financially sustainable.
“That’s the challenge we must solve if we are to meet the demand for lifestyle medicine that is growing among patients tired of the ever-increasing quantities of pills and procedures and their associated rising costs. We can’t afford to sit on the sidelines as the crisis of preventable chronic disease and the associated cost — both in human suffering and dollars spent treating these conditions — continue to rise.”
A sense of urgency
The current trajectory of health care spending in the U.S. is unsustainable.
A 2021 Government Accountability Office (GAO) report concluded that the toll of preventable chronic health conditions in the U.S. is high and might worsen if current trends continue. A 46 percent rise in severe obesity in just a decade “could be a bellwether” for increases in other chronic health conditions and related deaths, the report stated.
Government spending, including Medicare and Medicaid, to treat cardiovascular disease, cancer, and diabetes accounted for 54 percent of the $383.6 billion in health care spending to treat these conditions, the report found.
Lifestyle medicine is the use of evidence-based lifestyle therapeutic intervention — including a whole-food, plant-predominant eating pattern, regular physical activity, restorative sleep, stress management, avoidance of risky substances, and positive social connection — as a primary modality, delivered by clinicians trained and certified in this specialty, to prevent, treat, and often reverse chronic disease. Since the American Board of Lifestyle Medicine and ACLM launched the first certification exams in 2017, the total number of certified diplomates has grown to nearly 2,800 in the U.S.
It is proven that intensive and personalized lifestyle interventions can successfully treat, prevent and even reverse many diseases such as obesity, diabetes or heart disease. Yet clinicians who practice lifestyle medicine face confounding puzzles of how to code diagnoses and interventions to receive reimbursement from an insurer or other payer, according to Catherine Collings, MD, FACC, MS, DipABLM, director of Lifestyle Medicine for Silicon Valley Medical Development and El Camino Health Medical Network and president of the American College of Lifestyle Medicine.
Coding for lifestyle medicine interventions is wildly inconsistent treatment of patients with diabetes, hypertension, heart disease, hyperlipidemia, obesity and other conditions, she said.
“There are two entangled issues: Patients cannot get the care they so desperately want and physicians and other qualified lifestyle medicine team members cannot get the reimbursement they deserve,” Dr. Collings said. “Lifestyle medicine interventions are most effective with a team approach where the physician pulls in the expertise of a nutritionist, exercise specialist, or health coach when appropriate. Yet the number of patients who are eligible for medical nutrition therapy is severely restricted.”

Knowing what her patients eat and do not eat is the number one risk for progression of their disease, according to the Global Burden of Disease Report. A referral to a lifestyle medicine trained nutritionist can be life-changing for patients, so it is maddening for reimbursement barriers to stand in the way.
“My exercise physiologist had no CPT codes to seek reimbursement, even though exercise can be a dramatic intervention in chronic disease treatment,” she said. “My health coach had no CPT codes to reimburse her invaluable service to patients. In a country seeing rising lifestyle-related chronic disease, to handcuff lifestyle medicine physicians and their patients is akin to shutting down the fire departments and handcuffing the firefighters in yearly California wildfires.
“If we tried to use an across-the-board coding strategy ignoring these eligibility hurdles, there are a couple things that could happen,” Dr. Collings said. “The patient could get surprise billing and be very unhappy. We will get audited, which is a lot of work for our billing department staff who now must spend their time providing more and more documentation to justify it.”
Even if the reimbursement attempt is ultimately successful, the time the office staff spends pursing it often costs more than the reimbursement is worth, she said.
“It would be worth it on a big procedure if you’re seeking a $3,000, $5,000 or $10,000,” Dr. Collings said. “But lifestyle medicine itself is not high revenue in the first place. What are you likely to do? Throw up your hands and bill for the bare minimum that you know is covered and do the rest pro bono.”
Invest in the future
In the research publication on reimbursement barriers, survey respondents echoed those frustrations and shared specific examples of barriers, including a Medicare patient who was denied coverage for a nutrition-focused weight management program in favor of a costlier surgical procedure, as well as receiving warning letters from insurance companies when patients’ medication prescriptions are de-escalated following lifestyle medicine treatment due to a decreased need for drugs.
The Clinical Practice and Value Committee comprises about a dozen experts and is still in its early stages. Among the complex topics under discussion are facilitating reimbursement for lifestyle medicine services, establishing relevant quality measures and creating a clinical data repository for lifestyle medicine. The committee must remain flexible and adjust in real-time to ever-changing health reimbursement guidelines, Dr. Patel said.
Her hope is that her donation to seed the committee’s work will inspire fellow clinicians to help financially support the project to enable its goal of establishing a sustainable model for the integration of lifestyle medicine.
“I think of it as an investment in our own future,” Dr. Patel said. “There so many health care professionals who know lifestyle medicine is often the best medicine for their patients, they just don’t know how to provide it and keep their practice financially viable.
“Let’s solve this problem together.”