Lifestyle medicine for all: Interventions for treating chronic disease in under-resourced patient populations
No matter practice type, advancing lifestyle medicine interventions for patient populations most at-risk for lifestyle-related chronic diseases is a priority for board-certified lifestyle medicine clinicians.
By Stacia Johnston
ACLM Director of Health Equity Advancement
July 11, 2024

Statistics continue to confirm that minority and lower-income populations are disproportionately impacted by the prevalence and negative outcomes of chronic diseases in this country. Undoubtedly, all people deserve access to lifestyle medicine but social drivers of health (SDoH) can place challenging limitations on historically underserved communities who could benefit from lifestyle medicine interventions. While SDoH factors fundamentally impede on some patients’ ability to live a healthy lifestyle and even access evidenced-based lifestyle medicine, the unfortunate assumption is lifestyle medicine is only for the wealthy. In reality, ACLM members are working successfully within various types of practice settings across the U.S., including community health centers, to provide lifestyle medicine to some of the nation’s most under-resourced patients.
Examples continue to emerge and be documented as innovative models to improve health outcomes for underserved patient populations. For example, the Eliminating Barriers Initiative at Northwell Health is a program designed for underserved patients in New York who are living with diabetes and experiencing food insecurity. This model and many other examples confirm that lifestyle medicine application in diverse, low-income populations is attainable via collaborative, multistakeholder, and community-engaged multi-pronged approaches.
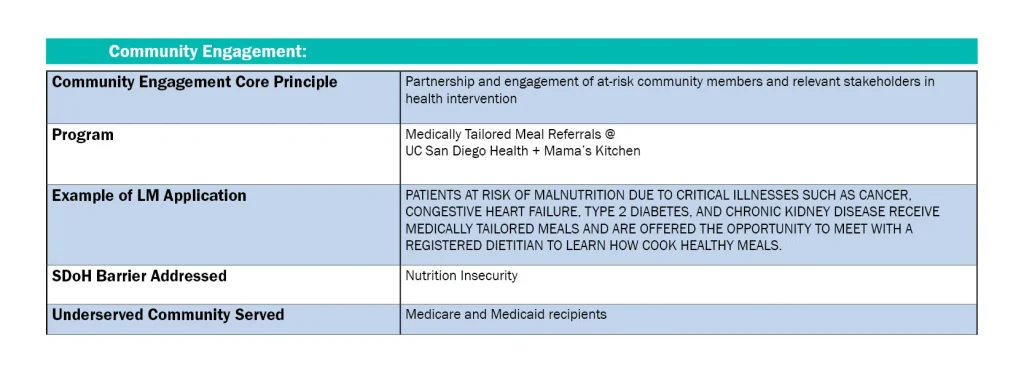
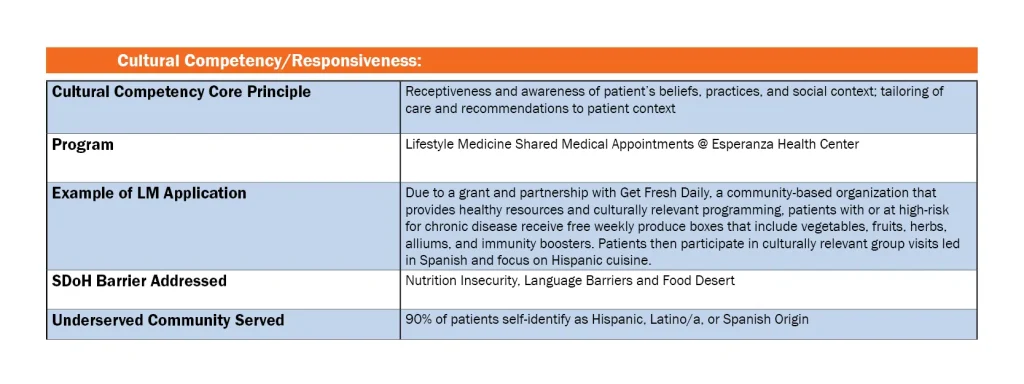
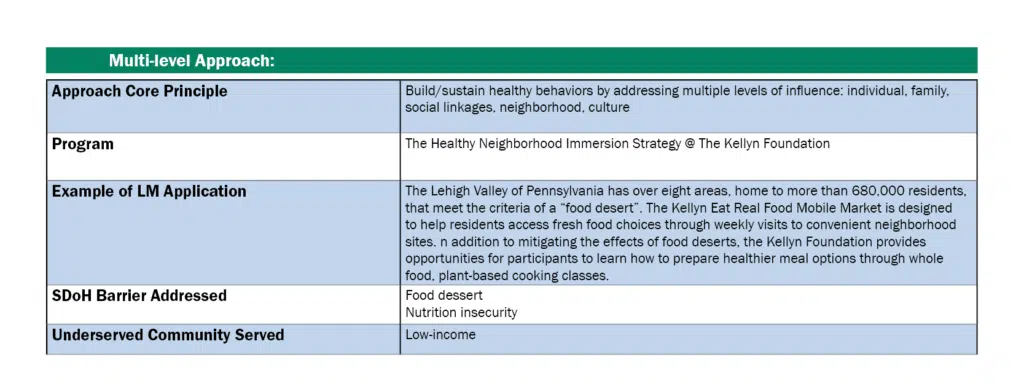
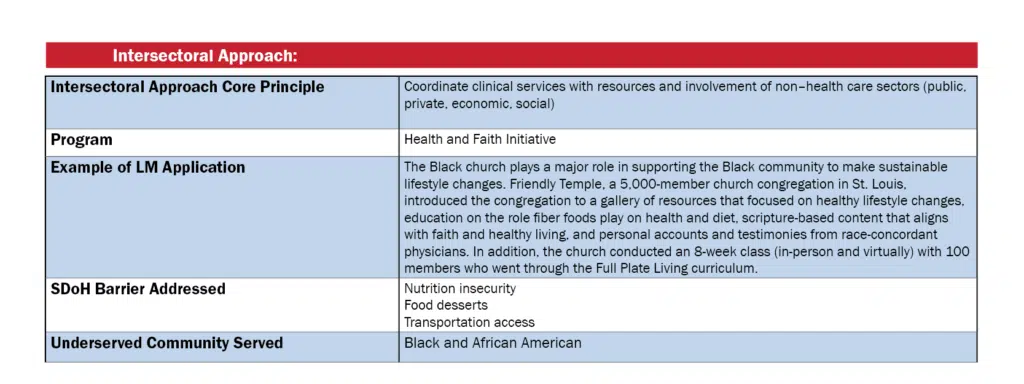
According to research, the community-engaged lifestyle medicine (CELM) model is an evidence-based, participatory framework capable of addressing health disparities through lifestyle medicine. Many care settings successfully deliver lifestyle medicine using this approach through its four key principles: community engagement, cultural competency, and application of multilevel and intersectoral approaches. Highlighted below are examples of how lifestyle medicine is achievable for under-resourced patient populations through those framework principles:
These brief examples are only a few that showcase appropriately tailored lifestyle interventions offered to all patients regardless of their income status or zip code. With any medical specialty, lifestyle medicine included, limitations do exist. However, ACLM and our dedicated members strive to support patients no matter what their barriers are.
ACLM established the Health Equity Achieved through Lifestyle Medicine (HEAL) Initiative to address lifestyle-related chronic disease health disparities with lifestyle medicine solutions. While we are not experts on mitigating the impacts of SDoH, we support our members in finding solutions to these challenges through this Initiative and its companion scholarship program, and other strategic partnerships with organizations aligned with our health equity efforts.