Research indicates that a plant-based diet consisting of unrefined plant-based foods is the cornerstone of healthy longevity and may be the most important prescriptive tool to help patients achieve a longer life and better quality of life as they age.
Abstract
As the number of centenarians increases globally due to improved living standards and access to quality healthcare, efforts to improve quality of life through modifiable health behaviors are even more relevant for the lifestyle medicine (LM) practitioner. Avoidance of the chronic diseases that plague our society today prolongs life and circumvents premature mortality1–7 while also making living better, not just longer, possible. Research indicates that a plant-based diet is the cornerstone of healthy longevity and potentially the most important prescriptive tool to help patients achieve a longer life and better quality of life as they age.
Key points for practitioners
- Globally, populations that traditionally consume largely whole food, plant-based diets are where we find the longest expected average life spans, as demonstrated by the regions dubbed the “Blue Zones.”3,41,42
- Both an increased consumption of unrefined plant foods and a decreased consumption of animal and highly processed foods seem to contribute towards increased longevity and reduced mortality.3,41,42,53
- Whole food, plant-based diets are associated with lower mortality and other intermediate health benefits such as improved cardiometabolic health outcomes.1,54
- Existing evidence on plant-based diets and longevity can be communicated to patients as part of wellness counseling.
- Adherence to a healthy dietary pattern such as the Mediterranean and MIND diets is associated with slower rates of decline in cognitive performance, lower risk for cognitive impairment, and
- Overall lower risk of AD and dementia.55–58
- Overall, plant-based diets can support a higher quality of life as individuals age.37
- If patients express interest in trying a whole food, plant-based diet of some kind, it is helpful to share ACLM patient-facing resources and tools for practical guidance on plant-based eating.
Longevity in context
Medical and health professionals have two fundamental purposes: to sustain life and to relieve suffering. If they are successful, the net effect is an increase in human longevity and quality of life. Recent research has indicated that genetic predisposition likely accounts for only 15–30% of longevity;8 for instance, the Danish Twin Study established that only 20% of the average person’s lifespan is dictated by genetics. Other research suggests that under 10% of lifespan is driven by genetics.9 Thus, environmental and lifestyle influences play a large role in determining lifespan.10
In 2020, life expectancy from birth was 78.9 years for the total US population. In 1860 it was 39.4 years and had risen over the past 160 years largely due to the dramatic decrease in infant and child mortality rates in the late 19th and early 20th centuries.
Additionally, medical advancements, fewer wars, and organized efforts to control the spread of infectious disease, including widespread water and sanitation infrastructure and improved living standards, all contribute to longer lifespans.11 Today in developed countries, non-communicable diseases (NCDs) are collectively the major cause of death, most of which are lifestyle-related.12 Though both social inequities and the COVID-19 pandemic have made the continued rise more uncertain,13,14 life expectancy has roughly tripled over the course of human history. However, since 1970, the main driver of these gains in industrialized countries has been a reduction in death rates from cardiovascular disease and cancer, particularly among older adults and largely due to medical interventions.15,16
The number of individuals 80 or older will more than triple in future decades, reaching almost 400 million in 2050.17 This demographic shift presents clear challenges for health care systems. Though nutrition is recognized as important to overall morbidity and life expectancy, its impact on health has often been underappreciated within the medical community. A suboptimal diet is the main modifiable risk factor for NCDs, along with physical activity, alcohol, and tobacco use.18
Morbidity, mortality and diet
Both disease and longevity are associated with diet quality.5,19 The comprehensive Global Burden of Disease Report that examined the health effects of dietary risks in 195 countries (1990–2017) found that low fruit, vegetable, and whole grain consumption and, similarly, high red and processed meat consumption are currently among the main global risk factors for chronic disease.20 In 2017, 11 million deaths and 255 million disability-adjusted life years or DALYs were attributable to dietary risk factors. High intake of sodium (3 million deaths and 70 million DALYs) , low intake of whole grains (3 million deaths and 82 million DALYs), and low intake of fruits (2 million deaths and 65 million DALYs) were the leading dietary risk factors for deaths and DALYs globally.20 The Global Burden of Disease study is important because nutritional studies with total mortality as an outcome are uncommon, largely because the sample size must be extremely large and the duration of follow-up long. However, mortality as an outcome has unequivocal clinical relevance.21
Proper nutrition, including lower consumption of refined, calorie-dense, and animal-based foods alongside higher intake of nutrient-dense whole plant foods, may help prevent almost half of the cardiometabolic deaths in the United States and, as such, promote increased lifespan due to disease avoidance.20 Specifically, a plant-based diet has been shown to decrease risk of all-cause mortality, obesity, type 2 diabetes, and coronary heart disease while effectively improving nutrient intake. Such health-promoting diets filled with nutrient-dense, fiber-protective whole plant foods have also been shown to reduce the risk of metabolic syndrome and type 2 diabetes by about one-half. Additionally, the risk of coronary heart disease events may be reduced by an estimated 40% and the risk of cerebral vascular disease events by 29% among populations consuming a plant-based diet.22
Cognitive decline
Addressing the cognitive health of older adults is key to quality of life, particularly as dementia is now the fastest-growing epidemic in developed nations.23 Dementia, which includes Alzheimer’s disease (AD) and other neurological dysfunction of the brain is now a leading cause of both mortality and morbidity globally and the leading cause of mortality in the U.S.24 Though medical treatments have successfully reduced mortality in the last twenty years with treatment for chronic diseases such as diabetes, heart disease, and cancer, mortality from AD has increased by more than 123%.25 A diet containing flavonoids, specifically a daily 1/2 cup of foods high in flavones and anthocyanins such as berries and dark leafy green vegetables, may lower risk of cognitive decline by as much as 20%, according to one study.26 AD is not exclusively a genetic disease. Unlike other genetic diseases driven by chromosomal or other gene-related flaws like Down Syndrome or muscular dystrophy, AD appears to have multifactorial origins and is potentially related to the body’s ability to respond to stressors, including glucose and lipid dysfunction inflammation, and oxidation.27 Thus, a lifestyle approach to treatment is warranted to address these pathological pathways, particularly utilizing nutrition.
Elevated cholesterol and blood pressure appear to be associated with AD,28 as is saturated fat.29 Further, probiotics and antioxidants in plant foods can positively modulate the immune response by reducing gut inflammation and neurodegeneration.30,31 Accordingly, adherence to healthy eating patterns, including the MIND diet, a hybrid Mediterranean-Dietary Approaches to Stop Hypertension diet, has been associated with slower cognitive decline. In the MIND diet study, lower AD rates were observed at the highest tertiles of adherence to a plant-prominent diet (HR = 0.47, 95% CI 0.26, 0.76).32 More research has indicated that this dietary pattern shows promise to preserve brain health and for treatment to address AD, including research examining cholesterol,33 animal product intake,34 and NHANES data on cognitive health and insulin resistance,35 indicating that diet, a controllable factor in brain health, can modulate cognitive decline.
Quality of life
Healthy dietary patterns are associated with lower disease burden and mortality rates, as measured by disability-adjusted life years (DALYs). Cohort studies such as the large European Prospective Investigation into Cancer and Nutrition–Netherlands indicate that plant-based dietary patterns are associated with lower disease burden as reflected in DALYs.36 A 2021 Japanese review of DALYs found that vegetable consumption reduces a range of health challenges associated with mortality, including diabetes, kidney disease, and cancer. The use of medications to treat chronic disease can also add to disability and decrease life years.37 In fact, research has found that DALYs are inversely related to the increase of drugs launched for use. On an individual level, the number of prescription medications being taken is also implicated in quality of life. Studies on vegan and vegetarians show that plant-based eaters take fewer medications, including anti-hypertensive,38 asthma,39 and diabetes medications.37,40
Quality of life comprises a complete package of health and lifestyle factors as they relate to longevity and is well-illustrated by examining populations of older adults living long and healthy lives, such as the “Blue Zones” discussed below.
The “Blue Zones”
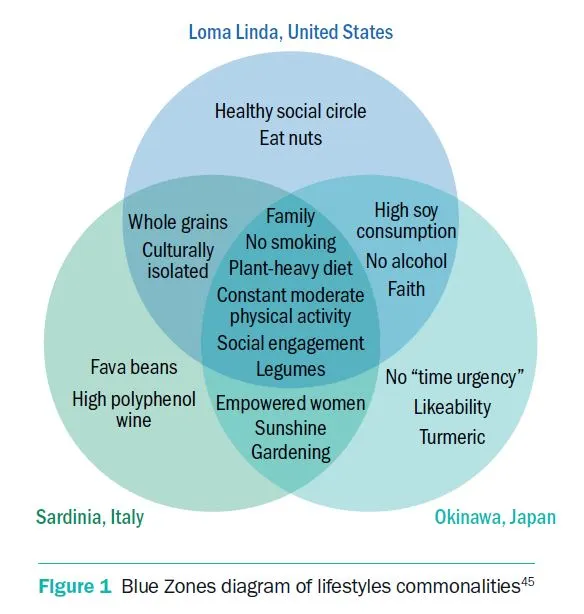
Plant-based dietary patterns are common among longer-lived populations, illustrated by those living in “Blue Zones,” a phrase coined by author Dan Buettner in his 2008 book to describe five places around the world where residents have the greatest longevity. His project aimed to find commonalities among them and found they shared particularly healthful plant-based eating patterns.41 The original Blue Zones identified included Okinawa, Japan; Ogliastra, Sardinia; Loma Linda, California; Ikaria, Greece; and the Nicoya Peninsula of Costa Rica. Though their lifestyles differ, they all share certain lifestyle traits that enhance and prolong their lives. They include diet, built-in routine exercise, social and familial connection, and living a purposeful life. The dietary component in all Blue Zones is primarily plant-based, (95%)42 with daily legume and local vegetable consumption, providing high levels of fiber and phytonutrients that protect against chronic disease. We will highlight three examples from the “Blue Zone” regions to identify the lifestyle practices that support longevity and illuminate their commonalities to better understand how modifiable lifestyle factors may be addressed within the scope of medical practice.
Okinawa
Among the common healthy habits are high levels of daily physical activity, positive attitude, and high consumption of fruit, wild plants, and vegetables, with minimal or no consumption of meat products. Interestingly, Okinawa, also Japan’s poorest prefecture, had the highest longevity indices in the country.43 In Okinawa, the traditional diet was plant-based and rich in phytochemicals and antioxidants. Over half of daily caloric intake came from sweet potatoes. They also consumed high amounts of green leafy vegetables and soy products while taking in minimal fat (about 6% of the total energy intake).21 Interestingly, in 1988, the daily intake of meat and pulses was higher than the national average, approximately 90 grams for each. This amounted to roughly 20% and 30% higher, respectively. Traditional daily intake of green and yellow vegetables was about 50% higher than the national average. However, by 1998, the global transition towards a preference for dietary meat had made its mark, and daily meat intake, as well as percent energy from fat had surpassed 100 grams and 30%, respectively, while daily intake of pulses and green and yellow vegetables had declined to the level of the national average.43 Today, longevity in Okinawa is no longer higher than the national average, but the net result of their relatively healthier diet on a global scale, along with modern technology, keeps them as a hotspot for longevity.
The lessons learned from Okinawa had major practical implications in Japan. Until the first half of the 20th century, life expectancy at birth was very low in Japan. However, within a short span of 50 years, thanks to major investments in public health infrastructure and nutrition education, the Japanese people now have the longest life expectancy at birth in the world.4 This example illustrates how fast change may occur and that dietary change paralleled positive shifts for public health.21
Loma Linda
Located in the orbit of Los Angeles is Loma Linda, California, where people live up to ten years longer than similar demographic groups in California.4 Much of this difference in lifespan may be attributable to dietary choices, including less meat consumption and more tomatoes, legumes, and nuts.4,6 Approximately 9,000 Seventh-day Adventists have thrived in this area following their faith’s endorsement of healthy living, which discourages the consumption of meat, caffeine, and rich foods. Smoking is also discouraged, and thus low rates of lung and other cancers and cardiovascular disease exist in this community. In 1958, a series of long-term medical research projects were started by Loma Linda University to study mortality and health among the Seventh-Day Adventists.44 From this longitudinal research, we have learned that nonvegetarian Adventists have twice the risk of heart disease than those following vegetarian diets, as well as higher risk for colon and prostate cancers.6 Dietary factors that may be protecting them include the high consumption of tomatoes which contain lycopene. Consumption is inversely associated with prostate, colon, and other cancers, as well as cardiovascular disease.46,47 Adventists consume higher quantities of nuts which may protect against cardiovascular disease.48 Further, water consumption is a principle of health for the Adventists, and the Adventist Health Study indicates that those who drank 5–6 glasses of water per day had a 60–70% lower risk of heart attack compared to those who drank considerably less in both men [relative risk (95% CI)=0.46 (0.28, 0.75); p trend = 0.001] and women [0.59 (0.36, 0.97)].49 Together, these practices may impact the overall health of the population.
Sardinia
The villagers of this rocky, hilly island have traditionally spent their days moving steadily to farm the land, shepherd their sheep, and tend to extended family. Though not necessarily strenuous, herders walk miles a day tending their flock.3 Other habits include a daily glass or two of Sardinian red wine, which contains high levels of antioxidants from the brightly-colored grapes used. The grapes produce more red pigment than most as a protection against the sun and are then allowed to marinate longer than most, resulting in two to three times the level of resveratrol, a flavonoid known to be atheroprotective.50 This compound has been shown to inhibit oxidation of low-density lipoproteins and their aggregation and to modulate cardiovascular disease.51 It also holds anti-inflammatory properties.51 Goat milk in this region, also a dietary staple, contains high levels of arzanol, an anti-tumor, anti-inflammatory substance found in the wild Sardinian dwarf curry that the goats graze on.3 Their cheese made from sheep’s milk contains high amounts of omega-3 fatty acids. Fava beans and chickpeas are consumed daily, and meat is reserved for Sundays or special occasions.3
Blue Zones lessons
Considering these regions of healthy longevity highlights the powerful effects of diet and lifestyle on life expectancy. Though these lifelong patterns play a role in disease avoidance, improvements in biomarkers can occur swiftly for those with chronic disease who choose to adopt these lessons. Particularly intriguing is emerging evidence that diet plays a major role in preventing age-related cognitive decline and Alzheimer’s disease. It has been shown that a diet rich in fruits, grains, legumes, vegetables, nuts, and seeds may cut the risk of Alzheimer’s disease by more than a half.32
Healthy aging and protein
Aging typically is associated with age-related reductions in muscle mass, function, and strength, the latter of which is termed sarcopenia. Sarcopenia results from numerous factors, one of which is inadequate dietary protein intake in older adults. Both nutrition and exercise interventions can delay this progression and enhance quality of life. Thus, recommendations for older adults emphasize sufficient, high-quality protein in their daily diet. Healthy older adults should aim to consume adequate protein: 1 to 1.2 grams of protein per kilogram of body weight daily—a 25% to 50% increase over the US recommended daily allowance.52 Though there is no evidence indicating benefits of animal-sourced protein, it continues to be the norm. Research indicates no significant difference between animal or plant protein sources for muscle composition and size in older adults.15 Meeting protein recommendations with plant foods is feasible and would convey a host of other health benefits. Additional benefits of more protein-rich plant foods for older adults include dietary fiber to support gut health and maintain healthy body weight, antioxidants and phytochemicals to reduce oxidative stress that contributes to aging and disease pathogenesis, and omega-3 fatty acids to support brain health.21
Mechanisms
Lower rates of chronic disease
Avoidance of chronic diseases including obesity, cardiovascular disease, diabetes, certain cancers, and respiratory conditions is a major contributor to health and longevity, and averting risk factors can circumvent early death.59 These risks include excessive caloric intake from the rich Western diet, which adds risk for weight gain, heart disease, and metabolic dysfunction.40,60 Sodium in processed foods adds risk for hypertension, adding a burden to the heart and increasing risk of heart failure and stroke,61 as do high blood cholesterol, saturated fats, and trans fats from animal foods, which appear to play a role in the development of atherosclerosis, the hardening and narrowing of the arteries, by adding fatty deposits in the blood and affecting blood flow.54,62–65 Research indicates that a plant-predominant diet has the potential to increase life expectancy by reducing risk for chronic disease.22 Mechanisms that lower risk factors include effective long-term weight loss for those suffering from overweight, which not only controls blood pressure and blood cholesterol66 but improves glycemic control to avoid metabolic disorders such as diabetes. Diabetes adds the burden of cardiovascular disease risk. Further, using plant-based dietary treatment does not add potential harm from medications or polypharmacy.22,66
The first large study investigating diet and lifestyle related to mortality was the Seven Countries Study launched in 1958 by Ancel Keys. It established a positive correlation among dietary fat, blood cholesterol, and heart disease. With hundreds of reports published, this study established the cardioprotective effects of the Mediterranean diet and the effects of various fatty acids on serum cholesterol.66 The Mediterranean diet was first categorized here as one that is high in cereal products, legumes, fruits, and vegetables; moderate in fish; and low in dairy and meat products. Olive oil was identified as the principal fat component.67 Adherence to this plant-predominant dietary pattern and healthy lifestyle was associated with a >50% lower rate of all-cause and cause-specific mortality [(Mediterranean diet HR, 0.77; 95% CI, 0.68-0.88), (moderate alcohol use HR, 0.78; 95% CI, 0.67-0.91), (physical activity HR, 0.63; 95% CI, 0.55-0.72), and (nonsmoking HR, 0.65; 95% CI, 0.57-0.75)].68 Regression of cognitive decline and heart disease, as well as reversal of cardiometabolic dysfunction, has been documented in older adults prescribed a whole food, plant-based diet5,21,22,69,70
The Framingham multigenerational study of residents in one Massachusetts town found similar implications for mortality in that increased cholesterol and elevated blood pressure increase risk of heart disease, and diet and exercise can reduce risk.71,72 Further, excessive caloric intake common in the Western diet overwhelms adipose storage capacity and disrupts glucose and insulin metabolism that can lead to insulin resistance and the diabetic state.60 This dietary pattern provides less fiber and more saturated fat, both associated with unfavorable lipoprotein concentrations and insulin control, as well as cardiovascular disease risk.73 Cardiovascular disease continues to be the leading cause of death and disease burden in the US and worldwide despite the tremendous decline in the Western world due to medical advancement.74–76
Individuals consuming plant-based diets have lower rates of overweight and obesity than those whose diets include meat and refined foods.77–80 Both obesity and diabetes have been shown to increase mortality risk by altering pulmonary mechanics, increasing inflammation, and increasing lung injury and malfunction.81 Further, diabetes and high blood pressure are the leading causes of end-stage renal disease, which is associated with all-cause mortality.82 The fiber and antioxidants found in plant foods could explain lower levels of systemic inflammation and oxidation found to be both cardio- and immunoprotective.83–85
Regarding reproductive cancers, dietary modification can significantly improve estrogen metabolism to decrease morbidity and mortality from cancer because estrogen triggers the proliferation of endometrial cells during the menstrual cycle. Over time, risk of cancer development may be increased by the division of DNA-mutated uterine or breast cells, increasing the chance of developing new, spontaneous mutations from carcinogens or radiation.86,87 Overall, the phytochemicals in plants reduce risk for cancer, as they are anti-inflammatory and protect cells from damage.88,89 For example, cruciferous vegetables have active components that may protect estrogen metabolism and inhibit lipid oxidation and carcinogenesis,90,91 including lignans in flaxseed that appear to lower reabsorption of estrogen in the lower intestine.87,92 These components found in plant foods protect against cancer.88,93,94
Common questions and concerns
Do older adults need more protein? How can they get enough on a plant-based diet?
Older individuals are slightly less responsive to anabolic stimulus to build and maintain muscle mass from the essential amino acids taken in from protein,95,96 which means they need more protein than older adults. Adults are advised to consume 0.8 grams of protein per kilogram of body weight, or 0.36 grams per pound which averages to ~51 grams of protein per day (based on weighing 150 pounds). Experts in aging recommend that older adults consume 1.0–1.5 grams of protein per kilogram of weight, averaging ~100 grams of protein (for 150 pounds). Most American adults consume ~100 grams of protein per day, which is roughly equal to or higher than the recommendation for the older adult population; therefore, a diet consisting of 15 to 20% caloric intake from protein is easily achievable to cover their needs.96,97 A goal for older adults’ protein intake is to approach the upper end of the acceptable macronutrient distribution range (AMDR) of 10–35% of calories, and specific requirements within this range depend on individual health status and activity level.98
Do people need to adjust their diets as they age?
Because the basal metabolic rate slows with aging, caloric needs generally decrease, though the amount of protein needed increases slightly with age. Natural changes in physical activity and body composition slow the body down with less demand on musculature and for energy intake. Further, older adults are at greater risk for all chronic diseases, and, thus, healthy lifestyle choices like diet quality are more important.99
Do older adults need supplements?
Though many adults over 65 take supplements as recommended by their physicians, only a fraction actually need them to address a deficiency.100 Ideally, adequate micronutrient intake can be achieved for older adults from a healthy diet.101 Older adults do have some special dietary needs to maintain optimal health. Exceptions may include vitamin B12 and D. The need for supplementation should be considered under the advisement of a healthcare practitioner based on actual needs or clinical deficiencies as identified with bloodwork. Healthy bone density is important for older adults, and adequate minerals and vitamins needed for bone formation and mineral storage is necessary. Weight-bearing exercise may play a more important role for older adults who have adequate calcium, phosphorus, and caloric intakes that reflect adequate diet quality with antioxidants and phytochemicals coming from whole plant food.102
Do older adults need fish for healthy fats to ward off cognitive diseases like Alzheimer’s?
A healthy Mediterranean or plant-based diet emphasizing fruits, vegetables, whole grains, as well as sources of unsaturated fats like flaxseed, walnuts, soybeans, and possibly fish and olive oil has been shown to ward off age-related processes that could lead to cognitive decline.32,69,103 The benefits seen from including fish as a high source of omega-3 fatty acids could be due to the essential nutrient itself, which has anti-inflammatory properties and is important for cell signaling, not necessarily the dietary source of omega-3 fatty acid, as plant-derived omega-3 fatty acids have been shown to be protective, as well.104,105 Omega-3 supports the healthy colonies of gut microbes, decreases risk for high blood pressure, and limits oxidative stress to avoid systemic neuroinflammation.32,85,106 These benefits can be obtained by consuming any dietary source of omega-3 fatty acids104 such as flax or chia seeds, walnuts, or soy products. Gut microbes have been found to play an important role in the brain and nervous system.106–108 Though a higher intake of fish has been associated with lower risk of Alzheimer’s disease,109 it may be due to an increased ability to absorb fat-soluble antioxidants coming from fruits and vegetables in the diet, particularly carotenoids, that protect the omega-3 fatty acids in the brain from oxidation.110 The inclusion of fish for omega-3 fatty acids is not essential, and there are several plant sources to choose from, including those mentioned above.
What if an older adult has trouble cooking or eating?
For those with chewing and swallowing difficulties, very soft, well-cooked vegetables and grains may help improve consumption to enable sufficient nutrient and fiber intake through eating. If needed, enteral nutrition can provide the calories and nutrients for older adults who cannot meet needs from dietary sources. Plant-based formulas, with their inclusion of fiber and avoidance of refined sugars, are readily available and can provide optimal nutrients and calories with few risks, thus providing a good alternative or supplement to limited eating.111–113 These can also serve as meal replacements when cooking is not possible.
Summary of key studies
There is a large body of research on the relationship between plant-based diets, mortality, and longevity, especially focusing on cognitive decline. However, few studies focus on quality-adjusted life years (QALY) or quality of life, derived from following a plant-based diet compared to a standard diet. We have summarized the strongest studies from our literature review of plant-based diets and longevity in Appendix Table 1. Studies covered cognitive function (n = 2),114,115 all-cause mortality only (n = 2)116,117 and multiple causes of mortality (n = 5).7,118–121 Studies examining cognitive function and decline had mixed results. One study with participants in Quebec and France found no association between empirically derived dietary patterns and cognitive decline. Patterns defined by high plant-food consumption had higher cognitive performance at baseline, while Western-style diets showed lower baseline cognitive performance.114 However, this may be due to differing lifestyle factors. Another study on cognitive decline found cognitive performance differed across certain diets, including the Mediterranean, DASH (Dietary Approach to Stop Hypertension), anti-inflammatory, and MIND (Mediterranean-DASH diet Intervention for Neurodegenerative Delay) diets, with the MIND diet intervention producing cognitive performance 7.5 years younger than participants’ age would suggest.115 These findings suggest that multiple plant-based dietary patterns can promote cognitive well-being into old age.
Plant-based diets showed mixed effects in various causes of mortality. For all-cause mortality, five studies showed a decreased risk of mortality associated with plant-based diet patterns,7,116–118,121 while two studies found no significant effect.119,120 One study found decreased risk of pancreatic, lymphatic and hematopoietic cancers,118 while other studies found decreased risk of cardiovascular disease (CVD) and ischemic heart disease (IHD) associated with vegetarian or vegan diets.7,119–121 Substituting carbohydrate with plant protein and fat had a risk-reducing effect,120 while substituting with animal protein and fat had a risk-increasing effect for all-cause mortality, further supporting the link between plant-based diets and reduced risk of mortality.122,123
These studies show somewhat consistent disease risk and mortality reductions associated with plant-based dietary patterns, though regarding substantially large degrees of outcome heterogeneity based on race, study group, and population location emerged. In addition, men with higher plant-based diet scores seemed to confer greater benefits compared to women, suggesting that other lifestyle factors may be modifying the associations between diet and mortality risk.1 Further research should also focus on quality of life in the form of QALYs or disability-adjusted life years.
Promising results: Cases of improved longevity and quality of life
Healthy aging with a new lease on life
An 82-year-old man with a history of polypharmacy due to coronary artery disease, myocardial infarction, ischaemic cardiomyopathy, hyperlipidemia, hypertension, and persistent atrial fibrillation who presented with memory loss, cognitive impairment, fatigue, and weakness was given an exclusively plant, whole-food diet treatment, with moderate physical activity. Results reported include a rapid reduction of hyperlipidemia and high blood pressure and discontinuation of statin, anti-hypertensive, and beta-blocker drug therapies. The patient also reported reversal of impaired cognition and symptoms associated with atrial fibrillation and ischaemic cardiomyopathy, including light-headedness, fatigue, and weakness. This case demonstrates the exciting potential of dietary and lifestyle modifications to improve cardiovascular disease symptoms and reduce polypharmacy, along with associated negative consequences in older adults, particularly memory loss, which is so important to quality of life.124
After suffering two strokes within months, an 85-year-old man took on a whole food, plant-based diet to avoid further neurological and cardiovascular damage. Both his neurologist and cardiologist did not expect him to survive. As an accomplished athlete in his youth (semi-pro baseball, Golden Gloves boxer, and champion racquetball until age 85), he worked out every day until his debilitating strokes. His son, who cooked him every plant-based meal during his month-long rehabilitation, commented that the meals were nurturing, but the critical factor in his return to health was eliminating the dangerous foods that got him there. Almost a year after the first stroke, the man’s physical and cognitive skills improved daily. He graduated from his walker to a cane and enjoys daily scrabble games with “incredible” memory skills.125
Populations with exceptional longevity
Populations consuming plant-based diets appear to have exceptional longevity.116 For instance, the Blue Zones uncovered areas with high rates of people living into their nineties, including many living into their hundreds.126 Compared to the US, where life expectancy is 78.54 years (2018), life expectancy in Japan is 84.67, the longest in the world. Okinawa specifically has a very high prevalence of octogenarians. Among the 7th Day Adventist population in Loma Linda, CA, the vegetarian men and women have expected ages at death of 83.3 and 85.7 years, respectively. These are 9.5 and 6.1 years, respectively, greater than the general Californian population at the time of analysis (1985). Overall, greater adherence to a plant-based dietary pattern correlates with lower all-cause mortality, as uncovered by the EPIC-Elderly Study (European Prospective Investigation into Cancer and Nutrition),116 the Adventist Health Study2,7 and NHANES III data from the U.S.5
Conclusion
Though healthy longevity has shown to have a small genetic component, modifiable risk factors, particularly diet but also exercise, nonsmoking, and social connection, play a predominant role in longevity.67,68,127,128 Many examples of longest-lived communities exemplify these lifestyle factors and can help guide health practitioners in caring for and advising their patients. The dietary commonalities include a rich supply of antioxidants, fiber, other essential nutrients, and phytochemicals from unrefined plant foods in various forms.
CONTINUE READING IN THIS SERIES
Download the Full Series
Benefits of Plant-Based Nutrition
Get the full Benefits of Plant-Based Nutrition series in a single PDF — including in-depth footnotes and research references available only in the downloadable version. Perfect for clinicians, educators, or anyone who wants the full science behind the story.
Acknowledgement
This review was made possible in part due to a generous donation from Kate Farms. For more information on Kate Farms please visit their website here. www.katefarms.com