Practical strategies for using ACLM’s clinical practice guideline on lifestyle interventions to treat and prevent type 2 diabetes
In this blog post, CPG guideline co-author Dr. Meagan Grega offers a step-by-step example of how clinicians can use the guideline in the exam room to implement lifestyle interventions for type 2 diabetes, supporting patients in improving their long-term health.
By Meagan L. Grega, MD, FACLM, DipABLM, DipABFM
August 14, 2025

Type 2 diabetes (T2D) and prediabetes are alarmingly common in the United States, with over half of the adult population meeting the diagnostic criteria for one of the two conditions. In 2019, there were 38.2 million physician office visits for T2D, with diabetes of any type documented in 14.2% of all outpatient encounters. The annual cost for diabetes reached $413 billion in 2022, accounting for 25% of all healthcare dollars spent.
In response to the growing cost and healthcare burden of managing metabolic dysfunction, the American College of Lifestyle Medicine (ACLM) selected the treatment and prevention of type 2 diabetes and prediabetes in adults through lifestyle interventions as the focus of its first Clinical Practice Guideline (CPG). This CPG is not a comprehensive summary of how to diagnose or manage prediabetes or T2D, and it is not intended to replace other guidelines. Instead, it focuses explicitly on evidence-based lifestyle change interventions as the foundation of prevention and treatment of prediabetes and T2D. The goal of the CPG is to equip healthcare professionals with a robust suite of tools and resources that are directly applicable to the patients they care for every day. The critical next step is determining how to translate this guideline into action in the exam room.
Assessing baseline lifestyle habits
To explore this issue further, we’ll examine a real-world clinical scenario—one that reflects the types of patients many healthcare professionals commonly encounter.
Envision a female patient, age 62, with a history of hypertension, hyperlipidemia, obesity and osteoarthritis, who presents to your office to discuss her recent labs. She has had mildly elevated fasting blood glucose for several years, but now her labs are significant for a HbA1c of 7.5. She is understandably concerned about her new diagnosis of T2D and asks what you recommend as next steps in her treatment plan. How can the Key Action Statements (KAS) outlined in the CPG support your shared decision-making with this patient?
KAS 1 (Advocacy for Lifestyle Interventions), KAS 2 (Assessment of Baseline Lifestyle Habits), and KAS 3 (Establishing Priorities for Lifestyle Change) are excellent first steps in the discussion.
Highlighting the impact of healthy lifestyle behaviors in the treatment of T2D, including a whole-food, plant-predominant eating pattern, regular physical activity, prioritizing restorative sleep, healthy stress management strategies, nurturing connectedness, and avoidance of risky substances, is a powerful counseling tool. Patients are often familiar with the use of medications to manage diabetes, but may not be aware of the impressive outcomes that can be achieved through optimizing healthy lifestyle behaviors. When a healthcare professional actively promotes the importance of lifestyle change, it can have a lasting impact. Consider using Figure 3 from the CPG as a helpful patient handout to guide your discussion.
Assessing a patient’s current lifestyle habits provides a valuable baseline and supports future discussions about behavior change goals. There are several screening tools to consider in Table 8. Exploring the patient’s readiness to change is another essential component prior to creation of specific behavior change goals. Figures 4, 5, 6 are helpful patient handouts to utilize at this stage.
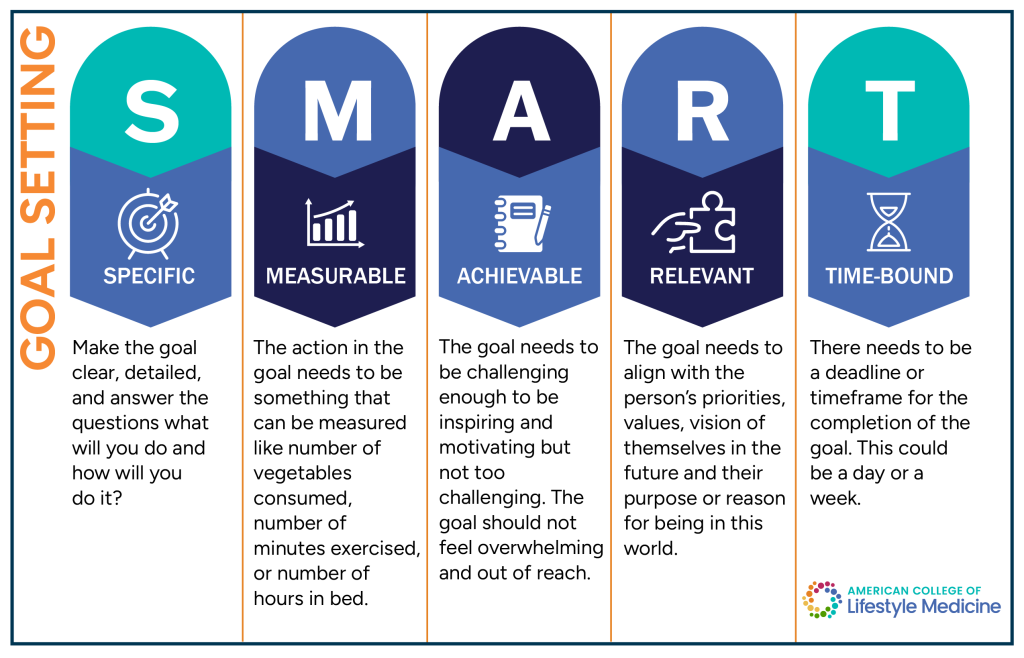
Engaging in shared decision-making regarding the patient’s goals and priorities is a critical step in the process. Using a “coach approach” to guide the patient in the creation of SMART goals (Specific, Measurable, Achievable, Relevant and Time-Bound) is an effective strategy for promoting patient autonomy, and sustainable change. Figures 7, 8 and 9 are helpful patient handouts to utilize during this process.
Crafting a lifestyle behavior change plan
OK – you’ve advocated for the importance of healthy lifestyle changes in the management of T2D, assessed your patient’s baseline lifestyle habits, explored their readiness to change, and introduced the concept of SMART goals. What next? KAS 4 (Prescribing Aerobic and Muscle Strengthening Physical Activity), KAS 5 (Reducing Sedentary Time), KAS 7 (Prescribing a Nutrition Plan for Prevention), KAS 8 (Prescribing a Nutrition Plan for Treatment), and KAS 11 (Tobacco, Alcohol, and Recreational Drugs) are helpful topics to explore as you continue to craft a management plan.
Achieving adequate physical activity and reducing sedentary time have a significant impact on blood glucose levels, in addition to improving cardiorespiratory fitness, sleep quality, cognitive function, and mental health. Figures 11 and 14, 15 and 16 are patient handouts to help guide the discussion, while Table 9 provides helpful physical activity resources specifically geared towards individuals with movement limitations.
The components of optimal nutrition are often an area of confusion for patients. In addition to referral to a dietitian, clinicians are encouraged to provide counseling on the benefits of a whole-food, plant-predominant eating pattern. An effective education strategy involves highlighting the consensus recommendations of multiple professional medical societies to follow a low-sodium, high-potassium dietary pattern that includes consumption of ample servings of fruits, vegetables, whole grains, and legumes (while limiting amounts of saturated fat, red meat and processed red meat, processed foods containing added sugars, sodium and refined grains, and sugar-sweetened beverages) as the preferred nutritional approach for supporting cardiometabolic health. Figures 18, 19, 20, and 21 and Tables 11-13 are excellent resources to guide shared decision-making in crafting nutrition SMART goals.
Alcohol, tobacco, and recreational drug use can negatively impact the management of T2D. Figures 26 and 27 are useful screening tools to utilize for patient assessment and counseling in regard to risky substance exposure.
Other lifestyle habits to address
Through motivational interviewing and shared decision-making, your patient has created SMART goals for physical activity, sedentary time, nutrition, and exposure to risky substances. What other lifestyle habits would be helpful to investigate? KAS 6 (Identifying Sleep Disorders), KAS 9 (Peer/Familial Support and Social Connections), KAS 10 (Identifying Need for Psychological Interventions), and KAS 12 (Achieving Person-Driven, Sustained Positive Behavior Change) are the next areas to consider. Check out Figure 17 (Lifestyle Sleep Health), Figure 22 (Relationships and Better Health), Figure 23 (Diabetes and Depression), Figure 24 (Managing Stress), and Table 21 (Practical Tips and Techniques Used in Behavior Change-Centered Interventions) for useful tools to guide your approach.
Additional considerations in the long-term management of type 2 diabetes include KAS 13 (Establishing a Plan for Continuity of Care) and KAS 14 (Adjusting Pharmacologic Therapy). Longitudinal relationships with a supportive team are the secret sauce of successful behavior change. Figure 29 provides a tool for patients to facilitate effective communication with their healthcare team. Deprescribing is another important area to evaluate in patients who are successfully making lifestyle changes while on diabetes medications. Figures 30 and 31 provide a structured framework for decreasing or discontinuing glucose-lowering medications in the context of lifestyle interventions.
Supporting patients in the treatment, remission, and prevention of diabetes is a journey. This CPG provides a roadmap to follow for encouraging behavior change as a foundational component of the clinical treatment plan.
About the author

Meagan L. Grega, MD, FACLM, DipABLM, DipABFM, is the co-founder and chief medical officer of Kellyn Foundation (www.kellyn.org), a 501(c)3 non-profit dedicated to making the healthy choice the easy choice. Through the “Healthy Neighborhood Immersion Strategy,” Kellyn provides school-based healthy lifestyle education and “garden as a classroom” programs; supports access to nutrient-dense produce via the Eat Real Food Mobile Market; engages participants in hands-on, plant-based cooking classes in community settings and offers intensive therapeutic lifestyle change interventions for families, employers, and community groups. She is a graduate of Bucknell University with a BS in biochemistry/cell biology and earned her MD from the University of Pennsylvania Medical School.