Addressing the physician shortage through lifestyle medicine
Burnout is driving more physicians to leave the profession and contributes to a growing shortage of primary care physicians. Lifestyle medicine can help.
By Sally Crocker
March 5, 2024

A lot has been reported about the stresses that physicians and other health professionals have faced in recent years. What the U.S. Centers for Disease Control and Prevention (CDC) calls a mental health crisis of burnout, work dissatisfaction, and demanding and sometimes dangerous job duties, is leading more healthcare workers to leave the profession.
In the last decade, the rates of burnout and dissatisfaction have doubled. The U.S. is running low on primary care physicians, according to the American Medical Association, with an estimated shortage of between 17,800 and 48,000 predicted by 2034.
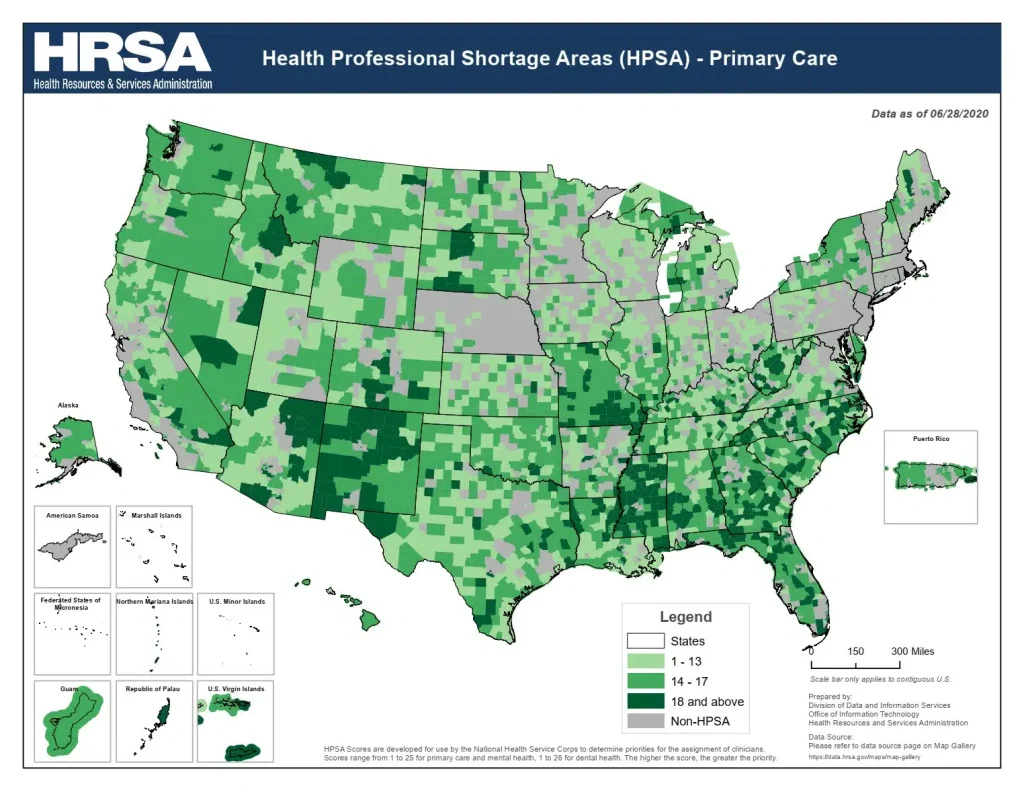
One report by the Association of American Medical Colleges (AAMC) says that more than 83 million people in the US live in a designated primary-care health professional shortage area (HPSA), and more than 14,800 practitioners are needed to remove the HPSA designation. The shortage of physicians can have negative consequences for patients and communities, such as delays in access to care, poorer health outcomes, higher costs, and lower satisfaction.
Since the COVID-19 pandemic, the healthcare industry has faced more stressors, further driving this shortage of primary care physicians. But the problem didn’t start with COVID, said Amber Orman, MD, DipABLM, who has served as Florida’s AdventHealth Medical Group chief wellness officer since 2021.
“Burnout has been a longstanding issue in healthcare,” Dr. Orman said. “Decreased productivity and increased physician turnover cost the industry around $5 billion a year.”
Burnout has grown over decades
Dr. Orman works with about 1,600 physicians and advanced practice providers to address challenges within the system and build solutions. Nationwide physician burnout surveys over the past few years reveal the primary drivers to be work overload, ineffective teams around them, lack of resources and autonomy, unhealthy work-life balance, mismatched values between employers and employees, not feeling their work has meaning, and lack of support from community, patients and coworkers.
“When you feel emotionally exhausted, that your work is not valued, it can manifest in decreased productivity and quality of care, patient dissatisfaction, higher medical errors and greater turnover,” Dr. Orman said.
Some clinicians are retiring early or working fewer hours. Others are entering different careers like medical consulting. The cost of replacing just one physician, depending on the specialty and practice, can be over $1 million.
This nationwide problem is so critical that it’s become a core initiative of the Office of the U.S. Surgeon General.
“The realities of our healthcare system are driving many health workers to burnout,” 21st U.S. Surgeon General Vivek Murthy reported. “They are at an increased risk for mental health challenges and choosing to leave the health workforce early. They work in distressing environments that strain their physical, emotional and psychological well-being. This will make it harder for patients to get care when they need it.”
Coping mechanisms
Burnout is not a simple problem to fix. However, there are coping mechanisms that help, said, Michelle Thompson, DO, DipABLM, FACLM, medical director for the University of Pittsburgh Medical Center’s (UPMC) Lifestyle Medicine Institute.
Dr. Thompson has incorporated culinary medicine and mind-body skills into her patient care while teaching medical students, interns, residents and attending UPMC physicians since 2006. She is leading the initiative to bring self-care to the center of patient treatment and employee health, and she is changing the way medical education and residencies are taught by placing lifestyle medicine at the center of training.
With a primary care office of her own, Dr. Thompson is also vice chief of staff for three UPMC hospitals and serves on the University of Pittsburgh School of Medicine physician well-being champion team, where she teaches mind-body, lifestyle and integrative medicine.
She emphasizes her own well-being, applying the six pillars of lifestyle medicine: a whole-food, plant-predominant eating pattern, physical activity, stress management, restorative sleep, positive social connections and avoidance of risky substances.
ACLM offers “Physician and Health Professional Well-being,” a course that supports health professionals in achieving and sustaining a healthy lifestyle. Like other healthcare organizations, AdventHealth also uses lifestyle medicine as a basis for the design of its physician and advance practice providers’ well-being program.
“During COVID we learned that we all have the same basic needs and can benefit from the six lifestyle medicine pillars,” Dr. Thompson said. “It creates joy for the physician to take time for self-care, pause from a full day of meetings to take breaks and move our bodies, fuel our bodies and take mindful moments. We have to take care of ourselves to be at our best for patients.”
Thompson has a treadmill desk in her office. She does yoga, takes nature hikes, lifts weights with a workout partner several days a week, and practices tai chi. She has eaten a whole-food, plant-based diet for over 32 years. She has incorporated artificial intelligence into her patient charting and transcriptions, trimming valuable hours of medical records time from her days.
“Through these tools, I gain balance and personal time to read a book, enjoy family and connect with colleagues,” she said.
Dr. Thompson isn’t alone. One study found that 90% of lifestyle medicine practitioners surveyed reported that lifestyle medicine positively impacted their professional satisfaction. They reported notable improvements in patient outcomes, increased patient satisfaction, and the development of more meaningful clinician-patient relationships as key benefits.
A successful patient and clinician
When patients are successful in their health journey, physicians and healthcare professionals feel more successful too.
An aging population suffering from chronic illnesses like cardiovascular disease, cancer, diabetes and respiratory conditions, are the most frequent and fastest growing population doctors treat. Simply managing these diseases through ever-increasing quantities of pharmaceuticals and procedures strips away the joy of truly healing patients. Lifestyle medicine certified clinicians are trained to apply evidence-based, whole-person, prescriptive lifestyle changes to treat and, when used intensively, often reverse many common noncommunicable chronic diseases.
“Lifestyle medicine is really at the root of everything we deal with, including chronic disease,” Dr. Thompson said. “When you implement lifestyle medicine into the patient visit and listen to your patient, you may find that the reason they have a weight issue is because of stress or lack of sleep, exercise or food choice. Every pill has side effects.
“People don’t want to take so many pills,” she said. “When the patient and physician work together to address the root cause of the problem, it can make an incredible difference.”
For clinicians interested in learning more about the practice of lifestyle medicine, ACLM in collaboration with the White House Conference on Hunger, Nutrition and Health committed to offer 5.5 hours of complimentary CME/CE in lifestyle medicine and food as medicine to 200,000 physicians and other health professionals until September 2025. Register here.
After physicians begin to administer lifestyle medicine to their patients, they often end up making many of the same changes with them, Dr. Thompson noted.
“The world will be a better place if we have happy and healthy physicians who can take better care of themselves and thus the world around us.”